How Does IVF Work?
A fertility specialist explains the process of in vitro fertilization, step by step, and what to expect.
About 97,000 babies were born in the United States in 2021 through in vitro fertilization (IVF) and other assisted reproductive technologies, with their use more than doubling over the past decade, according to the Centers for Disease Control and Prevention.
“IVF affords patients the opportunity to be parents in situations where they may never have been able,” says Dr. Alexis P. Melnick, a reproductive endocrinologist at the Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine at Weill Cornell Medicine and NewYork-Presbyterian. “It also gives patients choice and control over their reproductive timeline and decisions. Being able to be a part of these journeys is an incredible privilege.”
Dr. Melnick, who is also an assistant professor of obstetrics and gynecology and reproductive medicine at Weill Cornell Medicine, spoke with Health Matters to explain what to expect if you are considering IVF.

Dr. Alexis P. Melnick
What is IVF?
Dr. Melnick: IVF is the fertilization of an egg outside of the body in a lab to create an embryo. This embryo can subsequently be transferred back into a uterus.
When should someone see a fertility specialist?
A person should consider seeing a fertility specialist if they are under age 35 and have been trying to conceive for one year, or over age 35 and have been trying for six months. There’s no downside to seeing a specialist earlier if there are any concerns.
What do doctors check for?
The basic fertility workup typically includes:
- Bloodwork to check hormones, thyroid levels, and immunities, and infectious disease testing
- Ovarian reserve testing, which gives a sense of egg quantity
- An exam of the fallopian tube and uterus. This often includes a test called a hysterosalpingogram to evaluate the uterine cavity for conditions like polyps or fibroids, and the fallopian tubes for abnormal shape or blockages.
- Semen analysis
- Preconception genetic screening to see if the prospective parents are carriers of a genetic disease
Why might someone choose IVF?
IVF can be used for all kinds of fertility issues, including male infertility, such as issues with sperm count. In about half of all fertility cases, a male factor is a cause.
Female infertility can be caused by age-related infertility or by medical conditions such as endometriosis, fibroids, blockages in the fallopian tubes, polycystic ovarian syndrome (PCOS), or other problems with the ovaries. Sometimes there’s unexplained infertility, in which the work-up comes back normal.
IVF can also be an option for people who don’t have infertility. These include people who have had multiple miscarriages and want to test the embryos for a chromosomal abnormality, which can cause a miscarriage, or prospective parents who carry a gene for a disorder (such as Tay-Sachs disease) and want to test the embryo for the disease. Same-sex couples or people without a partner who want to have a baby, and women who want to freeze their eggs for the future, may also choose IVF.
How does IVF work?
The IVF process includes:
Medications and monitoring: As a first step, some patients may take birth control pills or estrogen patches to get the ovaries ready.
The patient will then take between one to three injected medications per night for 10 to 12 days. In a normal menstrual cycle, one egg grows. The self-administered injections stimulate your ovaries to produce multiple eggs. Another medication prevents your body from releasing the eggs too soon, so your doctor can retrieve them at the best time. During this stage, patients will come in frequently for bloodwork and ultrasound monitoring.
A final “trigger shot” matures the eggs in the ovary and gets them ready for retrieval.
Egg retrieval: About 35 to 36 hours after the trigger shot, the patient will undergo the egg retrieval, which is a surgical procedure done under IV sedation that can take about five to 10 minutes.
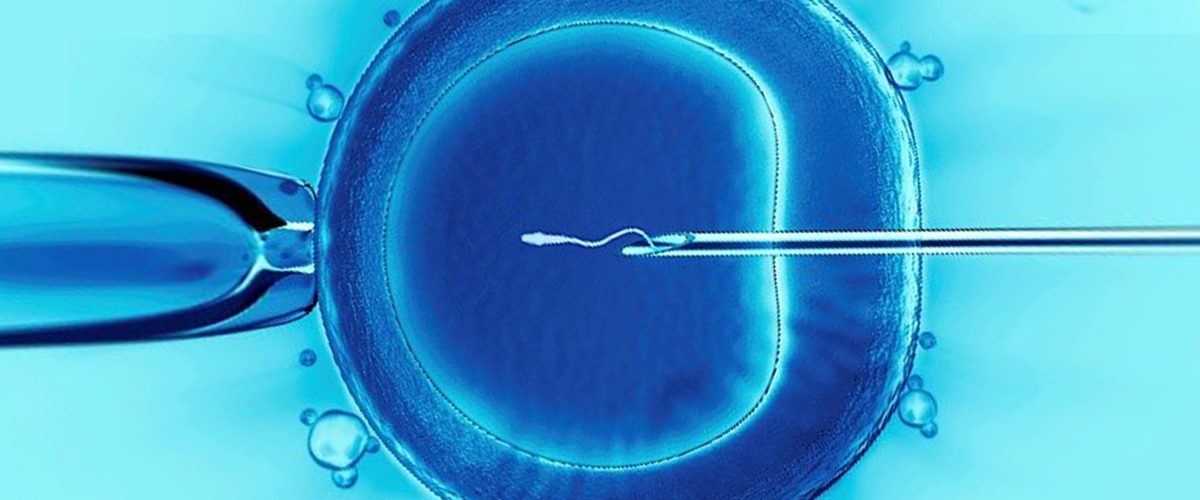
During the procedure, which is done through the vagina, an ultrasound probe guides a needle connected to a light suction device that withdraws the eggs from the ovaries. The eggs are then frozen for future use, if the patient has chosen that option, or brought to a lab for fertilization.
Fertilization: The eggs are mixed with sperm from a partner or donor. In certain cases, such as if sperm motility or counts are low, one sperm is directly injected into each egg.
Embryo transfer: An embryo can be transferred “fresh” three to five days after a retrieval, or frozen and then thawed and transferred in a subsequent cycle. During the transfer, a thin catheter is inserted into the cervix. A syringe attached to the catheter carries the embryo, which is then injected into the uterus.
When do patients know if they are pregnant?
After 10 to 14 days, a patient takes a blood test to determine pregnancy.
Is an IVF pregnancy high risk?
No, IVF itself does not make a pregnancy high risk. If there are other factors, like carrying multiples or underlying medical issues like high blood pressure, they will be considered high risk. But just having IVF does not make a pregnancy high risk.
How many IVF cycles are needed?
While about three IVF cycles is common, the number a patient goes through is highly variable and depends on the individual and their goals.
When a cycle yields a low number of eggs or the quality of embryos is poor, another round may not be recommended.
Some patients may want to test the embryos for a genetic disease or freeze embryos for the future because they’re not ready to have a child. In both cases, we’d want to make sure we have enough healthy embryos.
Even if a cycle is not successful, which of course can be discouraging, we’re learning from each one.
With my patients I try to be straightforward and say, “We’re going to make some changes moving forward. I think there’s a really good chance of this working,” or “I think we should start thinking about alternatives.”
It’s important to be upfront and open with patients throughout the process.
How effective is IVF?
IVF is not a guarantee, but every patient and scenario are different.
The success rates are dependent largely on age. It’s a huge range.
Conservatively, the highest rates of success for a live birth can be between 55% and 65% per embryo transferred for patients under 35, ranging down to under 5% for patients who are doing IVF in their early 40s.
The IVF process can seem very daunting, but it’s a very individualized process and there is a lot of support in place for patients.
Dr. Alexis P. Melnick
What role does age play?
Age is a huge factor. People talk about age 35 as if it’s this magic number, but you really start to see a drop-off in success rates in the late 30s. The slope of the curve starts to steepen around age 37 or 38, and from that point on, every year makes a difference.
That’s why we strongly recommend that patients be proactive if they decide they might want children later in the future. We’re seeing people freeze eggs much earlier, even in their late 20s.
While these numbers may seem discouraging, pregnancy in women over 40 is possible both naturally and with fertility treatment. It is always worth seeing a fertility specialist to discuss options.
Is IVF painful?
Overall, IVF is described as uncomfortable rather than painful.
Certain aspects like the nightly injections and bloating can be bothersome. Abdominal pain and cramping post-retrieval are normal but typically short-lived. Severe pain is rare and likely would indicate some type of complication. Most patients say they are pleasantly surprised by the experience.
What are common side effects?
Bloating, fatigue, and mild cramping are common after the procedure. The IVF medications can have side effects. The most common questions we get asked are, “How am I going to feel emotionally? Will my hormones be raging?” Some patients say they feel more anxious, moody, and teary, and others say they feel great and don’t notice a difference.
What are the risks?
Though the chance of these risks is small, they include:
- Bleeding and infection from the egg retrieval
- Ovarian torsion, or twisting of the ovary
- Ovarian hyperstimulation syndrome, in which the ovaries over-respond to the medications and become swollen
How much does IVF cost?
Depending on the location, IVF can cost between $15,000 to $30,000 per cycle.
Insurance coverage for IVF varies significantly, depending on the particulars of your plan and your location, as some states mandate coverage. Navigating the insurance landscape can be one of the most challenging parts of this process, so it’s important to understand your plan details early on.
What happens if it’s not successful?
If the embryos are good quality and it’s more of a uterus implantation issue, the embryos could be used in a surrogate, or gestational carrier. If it’s an egg quality issue, the patient could use donated eggs. For those who don’t want to consider egg donation or a gestational carrier, adoption is an option. And some couples say, “We’re going to keep trying on our own,” and we’ve seen cases where they do get pregnant.
How important is emotional support during IVF?
There are many emotional aspects of going through fertility treatment, being diagnosed with infertility, or undergoing fertility preservation. It can take a huge toll.
For many patients, this may not be what they thought they’d be doing, or it’s not their ideal scenario. It can be very stressful, and there is so much misinformation out there, which can make it more difficult. I encourage patients to connect with a psychologist, social worker, or psychiatrist if needed. Friends and support groups can also provide emotional support. Some patients may be prescribed medication to help.
The IVF process can seem very daunting, but it’s a very individualized process and there is a lot of support in place for patients.
Alexis P. Melnick, M.D., is board-certified in obstetrics and gynecology and reproductive endocrinology and is a member of the American Society for Reproductive Medicine. She offers patients a full range of reproductive services, including ovulation induction, in vitro fertilization, fertility preservation, oocyte donation and treatment of reproductive endocrinopathies and recurrent miscarriage, and menopause. Dr. Melnick is also a skilled surgeon, performing a variety of minimally invasive surgical techniques for treatment of endometrial and ovarian disorders.
Additional Resources
Learn more about fertility and reproductive medicine at NewYork-Presbyterian.
Read about AI-based technology as a new tool for embryo selection.
