Treating Endometriosis: What You Should Know
A gynecologic surgeon explains the signs and symptoms of endometriosis and how it’s treated.

Endometriosis is a common and chronic condition affecting one in 10 women and gender non-conforming people of child-bearing age. That translates to millions worldwide who live with the disorder involving abnormal tissue growth outside the uterus. Yet many women experience pain for years before seeking help, and the condition is often misdiagnosed.
“I’m passionate about this because I see patients with endometriosis every day, and the common theme is delayed diagnosis,” says Dr. Arnold Advincula, chief of the Division of Gynecologic Specialty Surgery at NewYork-Presbyterian/Columbia University Irving Medical Center. “It often ends up being about 10 years between the onset of symptoms and diagnosis. But it doesn’t need to get to that point. Delaying treatment is a missed opportunity to address a condition that could impair one’s fertility and quality of life.”
“We have women come into our center at NewYork-Presbyterian/Columbia University Irving Medical Center daily who finally feel validated for their painful symptoms,” he adds. “There is a huge amount of relief when there is a plan of action to treat them.”
For Endometriosis Awareness Month, Health Matters spoke with Dr. Advincula, the Richard U. Levine Professor of Women’s Health in the Department of Obstetrics and Gynecology at Columbia University Vagelos College of Physicians and Surgeons, about the signs and symptoms of endometriosis, how it is diagnosed, and how it can be treated.
What is endometriosis?
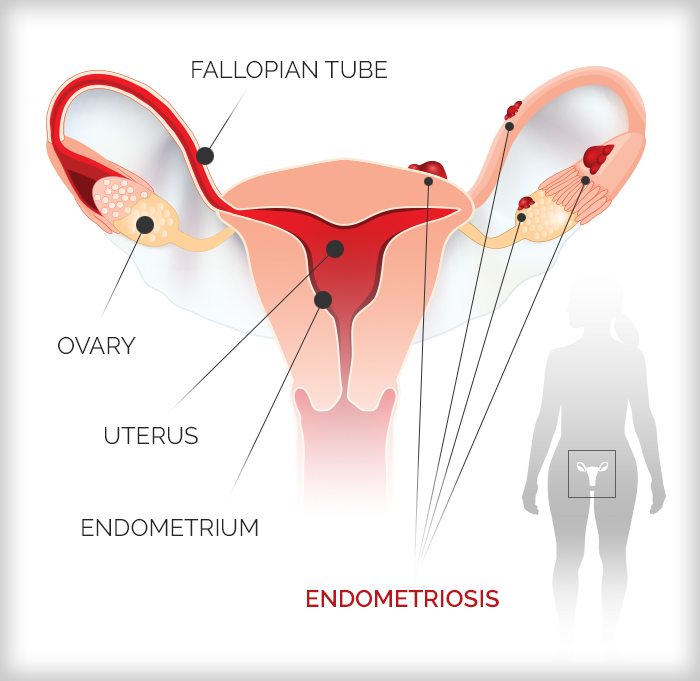
Endometriosis is a condition in which tissue similar to the endometrial lining — the tissue that lines the uterus and that menstruating women shed month to month — is found outside of the uterus in the abdomen or pelvis. When that tissue is found elsewhere it can cause chronic pain, inflammation, scarring, and can lead to infertility. It can also compromise other organs like the appendix, the bladder, and the small and large bowel if it spreads.
What are the signs and symptoms?
There are a lot of different ways that endometriosis can manifest and present. Bad menstrual cramps, painful intercourse, and infertility are the “trifecta” of symptoms. When we start to see women with those three complaints together, the index of suspicion is very high.
But we don’t always see all three of those things at the same time. Sometimes symptoms are subtle. Other times, people will have blood in their urine or stools or they will have painful bowel movements or pain with urination. Or they might have pelvic pain because they have an enlarged ovary from an endometrioma, a cyst that forms when endometrial tissue grows in the ovaries.
Now, these symptoms are not only specific to endometriosis because people can have painful periods and some of these other symptoms for other reasons. This is why it is often misdiagnosed. But when we examine the patient, consider their history of symptoms, and take the imaging into consideration, then we start to get a sense that maybe this patient has this disease.
How is endometriosis diagnosed?
The gold standard is minimally invasive surgery with laparoscopy, an outpatient procedure where we put a camera into a small incision in the belly to examine the pelvic organs. We can take a clinical history and do a physical exam, which can raise the index of suspicion very high based on findings and what we hear from the patient. But we can’t confirm it definitively until we do the surgery. We look for the implants — the evidence of the endometriosis in the abdomen and pelvis. We also look at the ovary and whether any cysts are present. Depending on what we find, we will then assess the best treatment plan.
"People need to know that there are clinicians who have expertise in this area and can help women who are suffering. "— Dr. Arnold Advincula
How is endometriosis treated?
For mild cases, treatment goals consist of managing symptoms and preventing progression of the disease. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help manage pain. Hormonal therapy can also help prevent progression.
If a person is not responding to medication, they may require laparoscopic surgery. That’s one of the best modalities to surgically correct endometriosis. It is often done with robotic assistance and only requires a few small incisions on the belly. If there is a cyst, we remove it; we excise — or cut out — the implants. Excision is often the best way to treat endometriosis. Sometimes we use what we call ablative therapy, where we essentially cauterize the implants. This combination — incision, ablation and cystectomy — is highly effective.
Surgery usually entails anywhere from three to five “bandaid incisions” on the stomach, and patients can go home the same day. Recovery time is typically two weeks; many women get back to work and life sooner than that.
What about more serious cases?
If endometriosis has spread to organs like the bowel or bladder, those organ systems may need to be operated on in order to remove the lesion(s). Sometimes people will need bowel resections, which is surgery to remove part of the small or large intestine, or an appendectomy, removal of the appendix. The last scenario — which you hope a patient will not have to go down this road — is a hysterectomy or removal of their ovaries because everything else has failed. However, in those complicated cases, surgery is quite transformative and dramatically improves a woman’s quality of life.
Can you get pregnant after surgery?
One of the main concerns women have is losing their fertility and loss of ovarian function. In other words, will treating endometriosis of the ovary affect their egg count? When we do endometriosis surgery, our ultimate goal for a patient who wants to get pregnant in the future is fertility preservation and fertility optimization. In the majority of cases, patients are able to successfully get pregnant and have children.
How does endometriosis affect fertility and pregnancy?
For women with endometriosis, the main hurdle is getting pregnant. When you’re trying to get pregnant in a pelvic environment that is inflamed because of endometriosis, it makes it very difficult. Endometriosis can affect the way the ovaries and the fallopian tubes function, which is necessary to connect sperm and egg. It can distort the anatomy in a way that makes it difficult to conceive. Sometimes women will need corrective surgery to correct the anatomy that’s been distorted by the disease in order to facilitate getting pregnant.
Once a person gets pregnant, endometriosis is not really an issue. Believe it or not, pregnancy is an excellent treatment because there’s something about the pregnancy state that addresses endometriosis and actually causes it to clear up and become inactive. Endometriosis does not affect the development of the baby or the delivery of the baby.
Typically, when a patient transitions into menopause, that’s often a positive thing from the endometriosis perspective, because at that point, the patient’s ovarian function is no longer able to stimulate the endometriosis implants. So we always hope for regression of the disease because the patient is in a menopausal state. It’s not going to progress like it does during a woman’s reproductive years.
Is there a cure for endometriosis?
There is no cure for endometriosis — it is a chronic condition that requires very thoughtful multi-disciplinary care. Surgery is one of the best treatment options. It’s important for women to understand that treatment must be balanced with a woman’s desires for future fertility and what she has in mind for her future goals. Every patient requires customized, personalized management of endometriosis.
Our team at the Endometriosis Treatment Program at NewYork-Presbyterian and Columbia are big believers in a holistic approach to managing patients with endometriosis. It’s not just about cutting out the disease. It’s about taking into consideration a patient’s concerns and wishes for the future. People need to know that there are clinicians who have expertise in this area and can help women who are suffering.
Arnold Advincula, M.D., is an obstetrician-gynecologist and chief of the Division of Gynecologic Specialty Surgery at NewYork-Presbyterian/Columbia University Irving Medical Center and chief of gynecology at the Sloane Hospital for Women. He is also the Richard U. Levine Professor of Women’s Health and vice chair of women’s health in the Department of Obstetrics and Gynecology at Columbia University Vagelos College of Physicians and Surgeons. Dr. Advincula is a leader in minimally invasive surgical techniques and gynecologic robotic surgery. Dr. Advincula has extensive experience in treating complex and challenging cases of endometriosis, uterine fibroids, and pelvic masses.
Additional Resources
Learn more about endometriosis management and treatment options at NewYork-Presbyterian.