What’s Causing Your Headache and When to Worry
An expert shares what to know about headaches, how to treat them, and when this common condition could signify something more.

Nearly every day, about one in 20 adults suffers from a headache, with a tension headache being the most common. But when is your headache “just a headache,” and when is it a sign of something more serious?
Health Matters spoke with Dr. Susan Broner, medical director of the Weill Cornell Medicine Headache Program, about what causes tension headaches, how to treat them, and when it makes sense to seek medical attention.

Dr. Susan Broner
Health Matters: What are the different types of headaches?
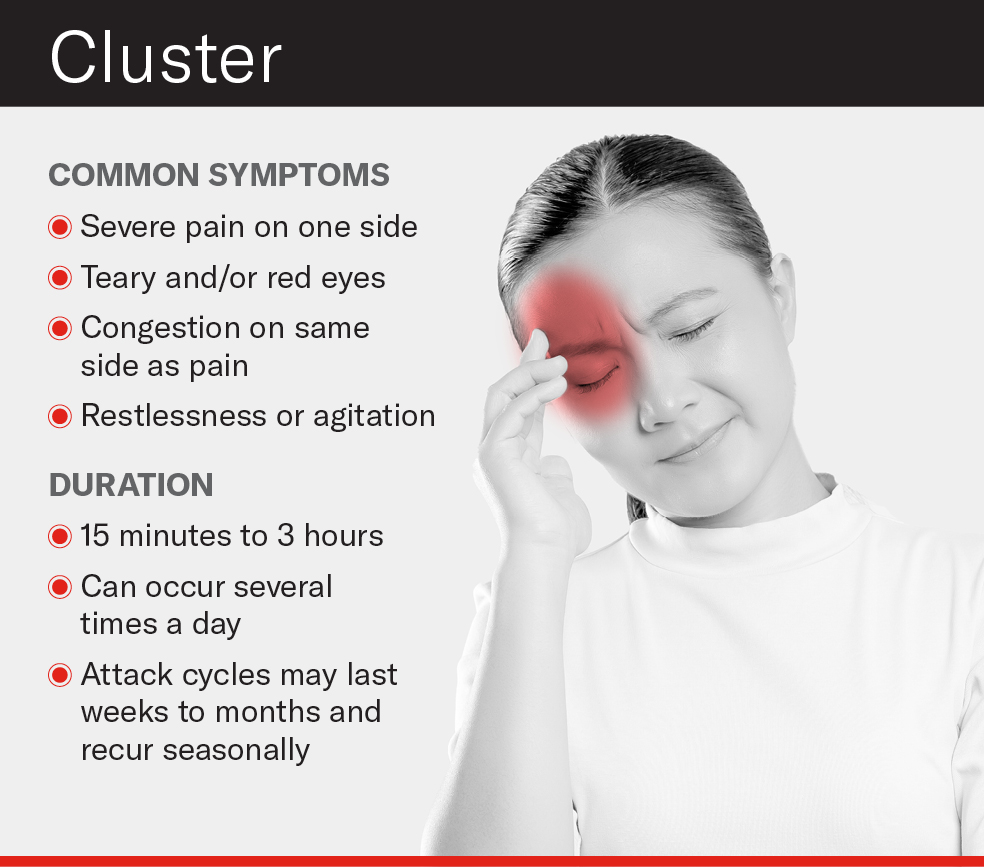
Dr. Broner: We divide headaches into two categories: primary headaches (like migraine, cluster headache, and tension-type headache) and secondary headaches. Secondary headache disorders are headaches that are caused by another underlying disorder that needs to be addressed — for example, a brain tumor or a sinus infection, or even a condition like Lyme disease.
Generally speaking, the kind of headache that people refer to as a “regular” headache is often a tension-type headache. The reason why we call it tension-type headache and not just tension headache is because it’s not just stress or tension that is the trigger.
Then what causes a tension headache, and what are the symptoms?
We don’t know exactly what causes tension-type headache — it’s the most common headache disorder, but the least understood. What we do know is that people who have them have muscle tenderness around the head, neck, and shoulders, also called pericranial tenderness. We don’t know if that’s a cause of headache pain or a reaction to it.
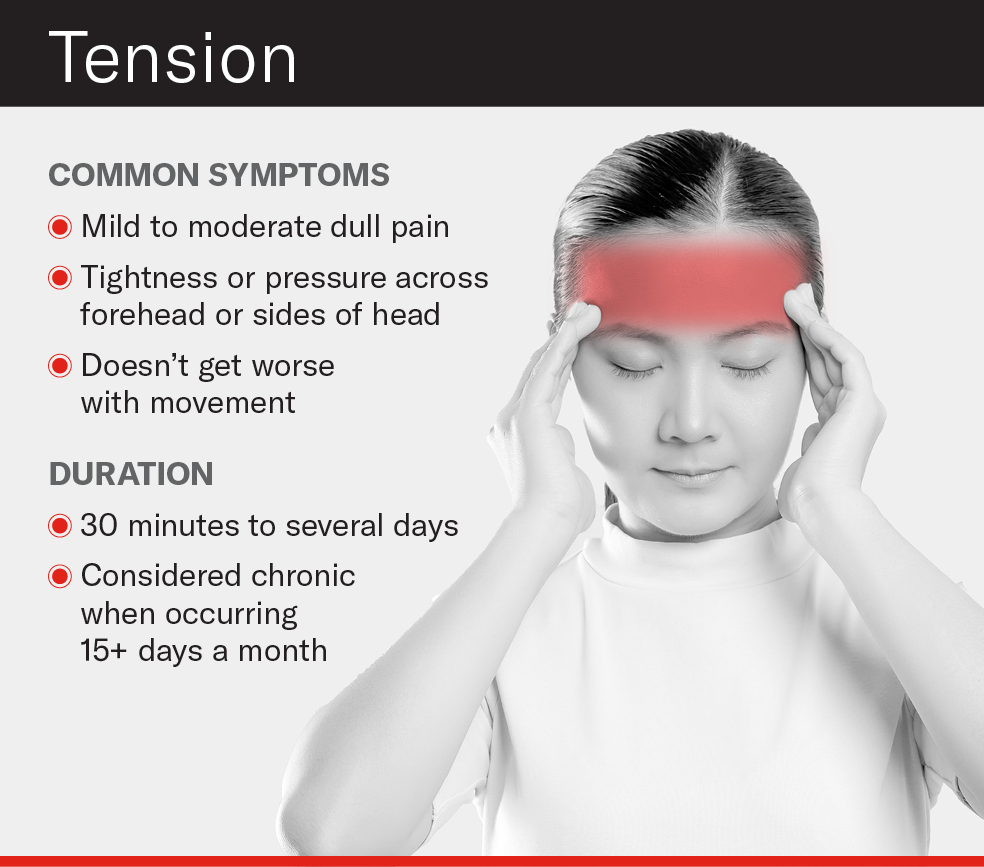
Stress and holding your muscles in a tight way can trigger a tension headache, but there may be other triggers like clenching your teeth, neck tightness, or neck disorders. The typical symptoms are dull head pain and tightness or pressure across the forehead or around both sides of the head.
How is a tension headache different from a migraine or cluster headache?
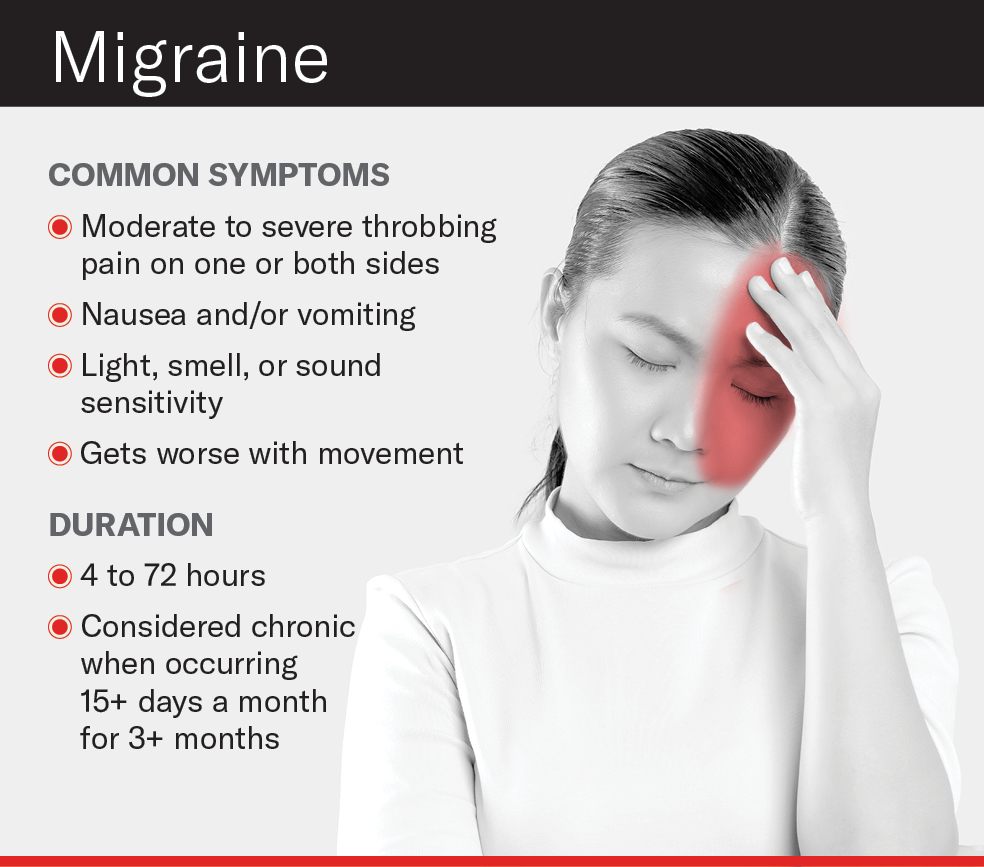
Tension-type headache is usually milder than migraine and cluster headache. Migraine headaches typically come with light and sound sensitivity or nausea, and throbbing pain on one side of the head. Tension-type headache can come with some light or sound sensitivity but none of those other characteristics.
Typically, a tension-type headache doesn’t interfere with day-to-day activities, unless a person has them more days than not. It can last anywhere from 30 minutes to a couple of days. Meanwhile, migraines last 4 to 72 hours untreated and can make it hard to think. Without treatment, they usually make people less productive or they can be debilitating.
How can you relieve a tension headache?
It usually responds to over-the-counter medicines like ibuprofen, aspirin, or Tylenol, as well as combined analgesics that contain caffeine. Just be careful not to use over-the-counter drugs more than two to three days a week regularly, because that could lead to more frequent headaches. For some the pain is mild enough that simple rest or a cup of coffee is enough.
For chronic tension-type headache, daily preventative medications may be prescribed. Some forms of antidepressants and antiseizure drugs, as well as biofeedback, have been shown to work well to reduce headache frequency. Speak with your doctor about what’s right for you.
What is biofeedback, and what other alternative therapies are available?
Biofeedback is a type of mind-body therapy that trains you to control certain body functions like your muscle tension, body temperature, or heart rate so that you can get into a state of relaxation. It’s one of the best treatments for a tension headache. Other complementary therapies like massage, physical therapy, and cognitive behavioral therapy can help you relax and ease the tension around the neck and shoulders.
Managing stress can also help with prevention. Stretching during the day, not overusing caffeine, getting enough sleep, eating regularly, working toward work/life balance — all of these habits can help.
When should you worry about a headache?
Any headache that gets progressively worse should be checked out by your primary caregiver. Also, if you’re 50 or older and start having headaches for no apparent reason, that’s a red flag — it could represent an underlying disorder.
Other warning signs that warrant contacting your doctor:
- You’ve had a headache for several days and it’s not going away
- Your headache starts to feel different or gets stronger (for example, a sudden explosive headache that feels like a thunderclap)
- Your headache keeps waking you up in the morning
- You experience new symptoms such as a fever or stiff neck
Call 911 and get immediate medical attention if you have stroke-like symptoms with your headache, such as:
- Blurred vision
- Sudden numbness in your face, arm, or leg, particularly on one side of your body
- Loss of balance or inability to walk
- Slurred speech or a sudden inability to speak
- Sudden confusion
- Dizziness
The bottom line: If your headaches are becoming more frequent, they aren’t going away, or you’re developing other symptoms, reach out to your doctor.
Dr. Susan W. Broner is an assistant attending neurologist at NewYork-Presbyterian/Weill Cornell Medical Center. She is also the medical director of the Weill Cornell Medicine Headache Program and an assistant professor of clinical neurology at Weill Cornell Medicine.
Additional Resources
Learn more about the diagnosis and treatment of headache disorders at NewYork-Presbyterian.
And for more on headache treatment programs, visit the Weill Cornell Medicine Headache Program or the Columbia Headache and Facial Pain Center.