New Treatment for Migraine Pain
A new nasal spray provides fast-acting relief for debilitating migraines. A neurologist explains how the medication works.

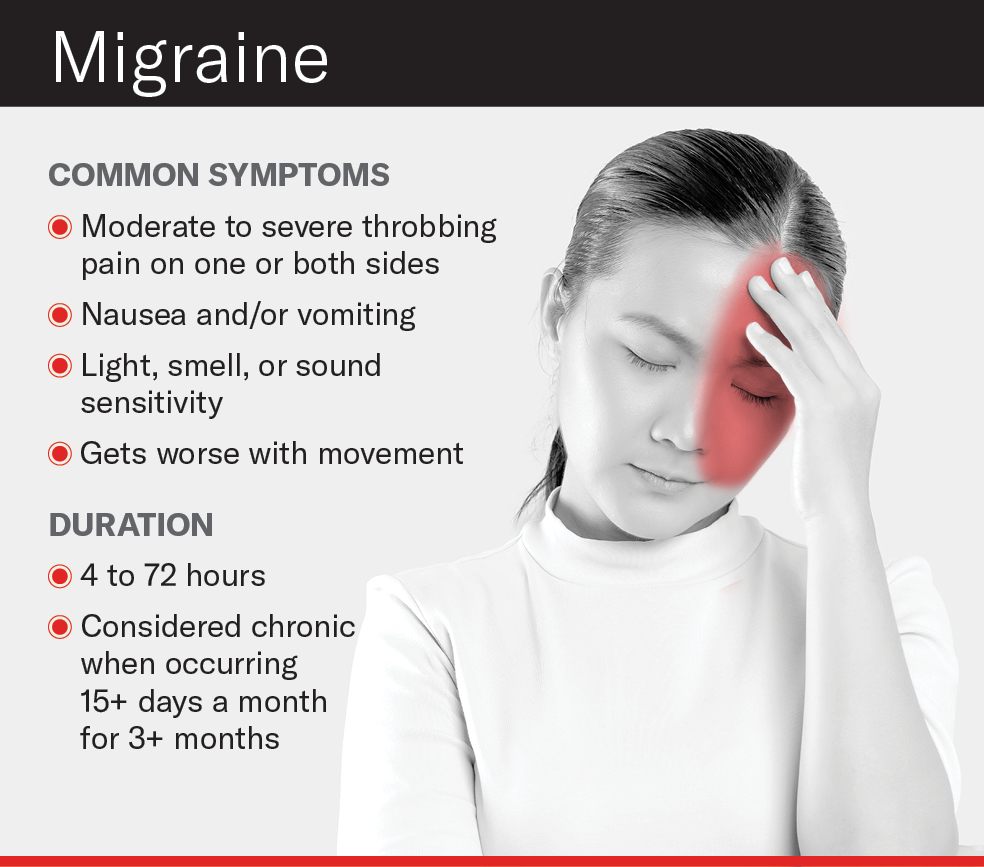
Migraines, those throbbing headaches that can last anywhere from a few hours to a few days, affect nearly 40 million people in the United States, according to the National Headache Foundation.
There are a number of medications on the market to treat migraine attacks and reduce their frequency, but a new prescription nasal spray called zavegepant provides fast pain relief for migraine sufferers, offering a promising new alternative for those who haven’t found relief from other migraine medicines. The FDA recently approved the new nasal spray, which is expected to be available in July.
“As a headache specialist, I’m always looking for a new nasal sprays,” says Dr. Susan Broner, a neurologist and medical director of the Weill Cornell Medicine Headache Program. “If someone has a migraine attack in the middle of the night where there’s vomiting and nausea, you would want a medicine that works as quickly as possible because the longer you have a migraine, the harder it is to treat. A nasal spray can act quicker than a tablet because it is absorbed more rapidly in the nasal cavity.”
Dr. Broner, who is also an assistant attending neurologist at NewYork-Presbyterian/Weill Cornell Medical Center, spoke to Health Matters to explain how this new medication works and what it means for migraine sufferers.

Dr. Susan Broner
What is the new medication and how does it work?
Dr. Broner: This nasal spray is part of a newer class of migraine medicines called gepants. They work by blocking calcitonin gene-related peptides, or CGRP, a protein released around the brain that causes inflammation and is believed to play a significant role in migraine pain. Gepants are already available in pills but now there is a nasal spray option that we hope will be faster acting.
How is it different from other migraine medicines?
The other main class of medicine for migraines is called triptans. They come in pills, nasal sprays, and injectables. Triptans tend to have more side effects, the most common being tight muscles in the neck, jaw, or chest, and fatigue. They work for a lot of people, but gepants are an effective tool for people who don’t respond well to or can’t tolerate triptans. The new nasal spray and other gepant drugs may also offer an alternative to people who, for medical reasons, cannot use triptans.
What are the benefits to a nasal spray versus a pill?
A nasal spray usually provides faster relief. Unlike pills, it bypasses the gut and is absorbed into the body faster, giving pain relief sometimes in as little as 20 to 30 minutes.
Migraine is not just a disorder of pain, but also light and sound sensitivity, fatigue, and nausea. For some people, the nausea would mean they might throw up a pill or it would not be well-absorbed. So having a nasal spray that bypasses the stomach is rather advantageous.
Is there a reason some people would prefer a pill to a nasal spray?
In my practice, most patients prefer a pill. They are easy to carry around, they are discreet and some people don’t like the sensation of a nasal spray.
Can this medicine help prevent post-migraine symptoms?
After a migraine attack, many people suffer from something called postdrome, sometimes known as a migraine hangover. It’s when a person feels crummy the day after having a migraine. Their pain may be gone but they still feel tired or they can’t think clearly. If you can knock the pain out early with the appropriate medication, you may be less likely to feel these prolonged issues. The quicker you get rid of the headache, the better you’ll feel, and you won’t miss so many days of work or school.
Would this medicine work for other types of headaches?
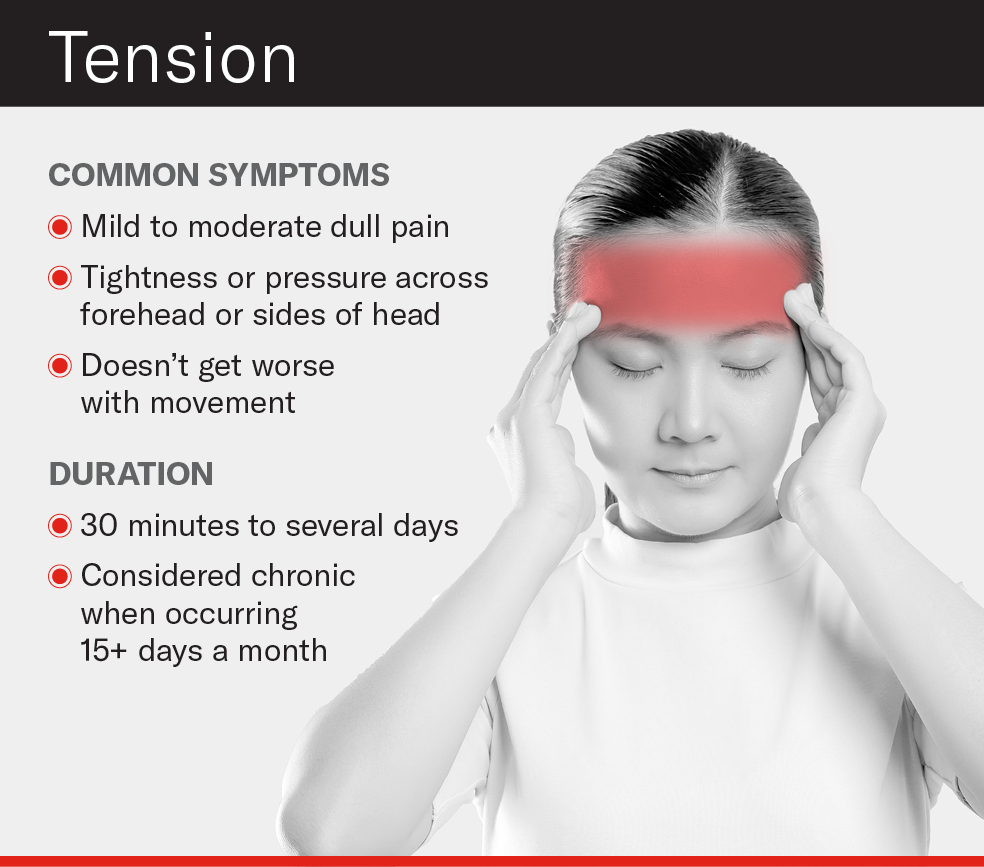
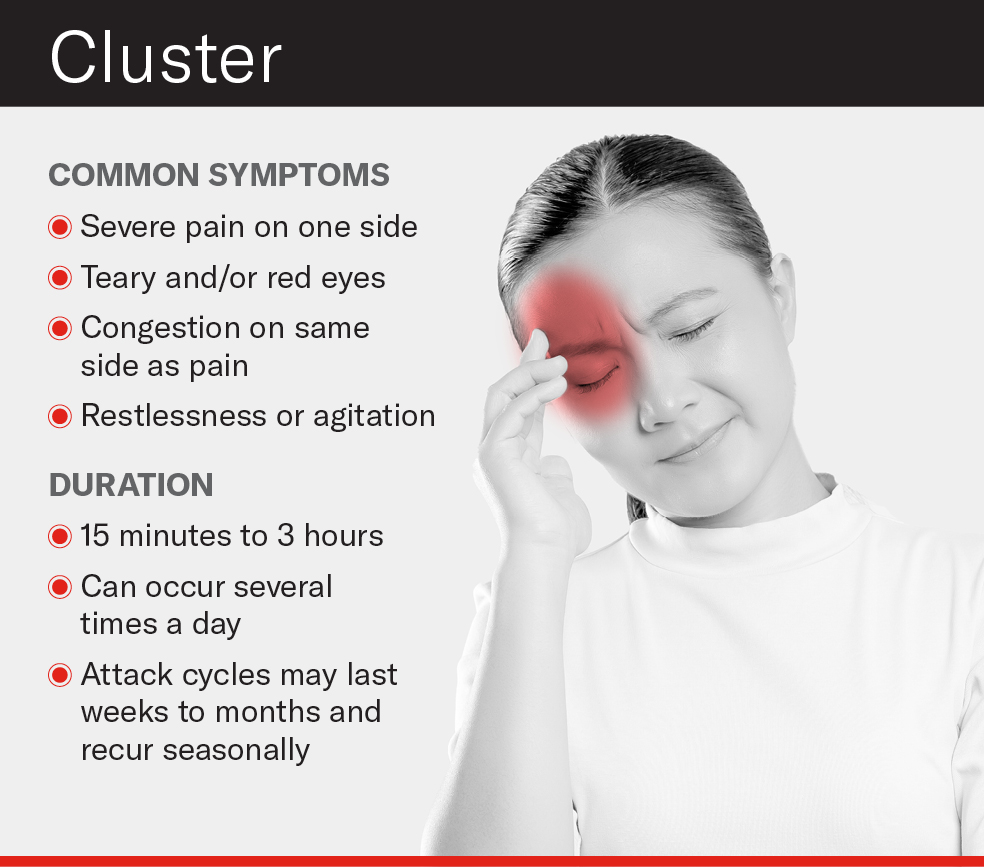
Right now the new nasal spray, and other drugs in its class, are only approved for use in migraine, not tension headache — the most common headache disorder — or cluster headache.
Does this medicine cure or prevent migraines?
We don’t have a cure for migraines, but there are medications that reduce migraine frequency. This particular medication is not a preventative but is used to interrupt a migraine episode. If you match people with the right medication and they catch the migraine when it’s mild before it gets strong, they may be able to nip the attacks in the bud and not be debilitated by them.
The gepant class of medications represents a step closer for us in understanding the underlying mechanisms of migraines. If we can find the earliest moment, biologically speaking, in a migraine episode, then maybe we can turn off a migraine before it starts. We’re not there yet, but we’re closer.
When Should you Worry about a Headache?
Any headache that gets progressively worse should be checked out by your primary caregiver. Also, if you’re 50 or older and start having headaches for no apparent reason, that’s a red flag — it could represent an underlying disorder.
Other warning signs that warrant contacting your doctor:
- You’ve had a headache for several days and it’s not going away.
- Your headache starts to feel different or gets stronger. (For example, a sudden explosive headache that feels like a thunderclap.)
- Your headache keeps waking you up in the morning.
- You experience new symptoms such as a fever or stiff neck.
Call 911 and get immediate medical attention if you have stroke-like symptoms with your headache, such as:
- Blurred vision
- Sudden numbness in your face, arm, or leg, particularly on one side of your body
- Loss of balance or inability to walk
- Slurred speech or a sudden inability to speak
- Sudden confusion
- Dizziness
The bottom line: If your headaches are becoming more frequent, they aren’t going away, or you’re developing other symptoms, reach out to your doctor.
Dr. Susan W. Broner is an assistant attending neurologist at NewYork-Presbyterian/Weill Cornell Medical Center. She is also the medical director of the Weill Cornell Medicine Headache Program and an assistant professor of clinical neurology at Weill Cornell Medicine. Dr. Broner’s research priorities include migraine in women, acute and preventative approaches, integrative headache care and identifying and addressing the needs of underserved populations.