What is Medulloblastoma?
A pediatric neuro-oncologist explains the rare type of cancerous brain tumor, why it is more common in children, and the options for treatment.
Source: National Cancer Institute
Medulloblastoma is one of the most common types of malignant brain tumors in children. It is a fast-growing tumor that forms in the lower back part of the brain, and there are approximately 350 new diagnoses a year. Recently, Good Morning America host Michael Strahan and his 19-year-old daughter Isabella shared that she has childhood medulloblastoma.
“Pediatric cancer is relatively rare, but we do see many brain tumors in our clinic and have several patients who are currently undergoing treatment for medulloblastoma,” says Dr. Luca Szalontay, a pediatric oncologist who specializes in brain tumors at NewYork-Presbyterian/Columbia University Irving Medical Center. “We always tell our patients and families when they first face the diagnosis that the goal is a cure.”
Brain tumors are the second-most common type of childhood cancer (after leukemia), and medulloblastoma accounts for 10% to 20% of all pediatric malignant brain tumors. Patients with medulloblastoma are typically first treated with surgery to remove as much of the cancer as possible, followed by radiation and chemotherapy.
Health Matters spoke to Dr. Szalontay to learn more about medulloblastomas and what it may mean for patients and their loved ones.

Dr. Luca Szalontay
What is medulloblastoma?
Medulloblastoma is a malignant brain tumor. It is the most common kind of ‘embryonal tumor’, which means that the cells that form the tumor are left over from fetal development. So the cause of the tumor has nothing to do with, for example, environmental factors or diet — it forms when there is a mutation in the cells that originate in the earliest stages of our growth.
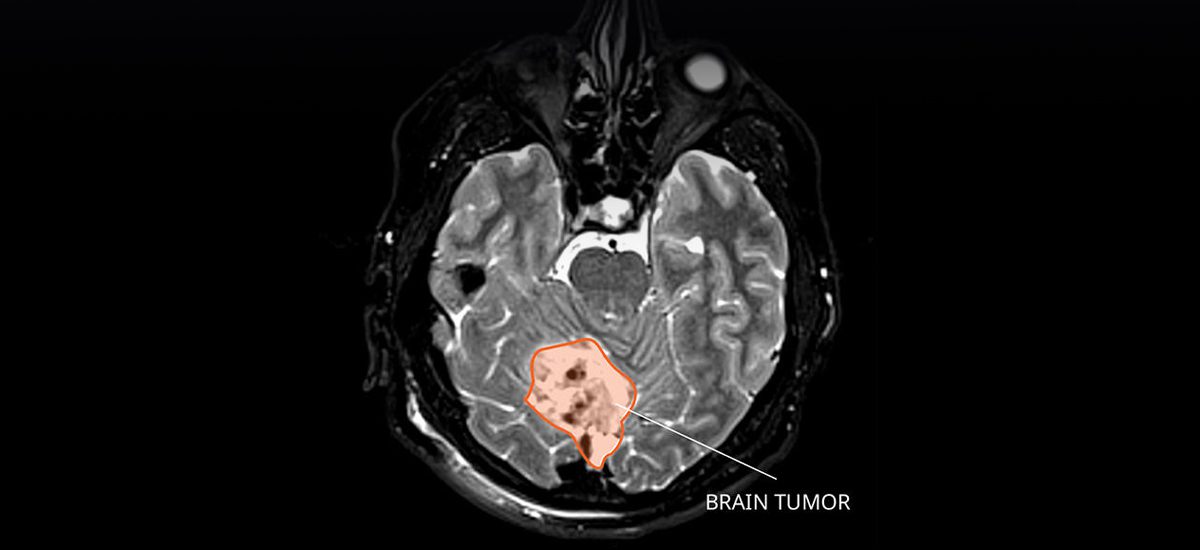
Typically, a medulloblastoma tumor forms in the cerebellum, which is the lower, back part of the brain between the cerebrum and the brain stem. It is a fast-growing tumor, and the cancer can spread outside the brain from the back of the brain to other parts of the brain and to the spine.
What does it mean when a tumor is malignant versus benign?
Malignant means that it is cancerous and growing very fast. When we look at malignant cells under a microscope, we see them dividing quickly. They usually have the ability to spread throughout the brain and the spine, oftentimes through the spinal fluid.
Benign means the tumor is non-cancerous. When we look at benign cells under the microscope, they usually resemble normal cells, and we only see a few of them multiplying or spreading.
How quickly does a medulloblastoma tumor grow and why?
Medulloblastoma is one of the fastest-growing tumors within brain tumors. Because a lot of cells are multiplying at the same time, it can double its size quite quickly. There is no exact time frame for its growth, but once it becomes symptomatic, the tumor is quite sizable by that time.
Who is at risk of medulloblastoma?
Children between 1 and 9 years old — the peak is around age 6. We do see adolescents and young adults with the condition as well, but it gets less and less common as someone gets older. It is also less common in young infants. In the pediatric world, about 20% of malignant brain tumors are medulloblastoma. In the adult world, only between 1% to 2% are going to be medulloblastoma, so it’s very rare in the adults.
What are the symptoms of medulloblastoma?
It depends on the child’s age and where the tumor is, and the symptoms may not appear until the tumor has grown. I would put the symptoms into two broad categories. First, if a tumor is growing in the brain, it is often blocking the flow of spinal fluid, which causes pressure in the brain. The symptoms are typically morning headaches, vomiting, and sleepiness.
Second, especially with medulloblastoma, there are symptoms related to its location in the back of the brain and brain stem. The cerebellum is responsible for coordination and balance, so it can impact our ability to walk. Other symptoms are numbness on one side of the face, paralysis, weakness, double vision, or slurred speech.
How is it diagnosed?
We do an initial visit and talk about the symptoms, and we do imaging tests. Oftentimes, we start with a CT scan, which uses a computer linked to an x-ray machine to take pictures. Later, we need an MRI (magnetic resonance imaging) to get detailed pictures of areas inside the brain and spinal cord. And a lumbar puncture is a procedure used to collect fluid from the spinal column. This is done by placing a needle between two bones in the spine and removing a sample of the fluid. A doctor will then check under a microscope for signs of tumor cells.
What are the treatments?
Surgery is the first step to take out as much as of the tumor as you safely can. The treatment depends on age of the patient. The reason is because, while radiation is effective against medulloblastoma, very young children are more likely to face long-term side effects.
For older kids, about 6 and above, our approach is to remove the tumor, then continue with radiation, and then finish the treatment with chemotherapy. With younger children, we start with surgery and do a higher dose of chemotherapy.
As time goes by, and we learn more and more about the disease, we are trying to tailor our therapy as much as we can and be successful in treating this disease.
What are the chances of recurrence?
If the cancer has spread, the recurrence rate is quite high. I would say more than 30% chance, even if we can eradicate it first.
How do patients typically do after receiving treatment?
If the tumor is localized, patients do well after treatment. We usually look at how patients are doing five years down the road and the survival rate is between 70% to 85%.
After we finish treatment, in the first year we see patients every three months, and we do an MRI every three months. In the second year, it’s every four months. And then in year three, four, five, it’s every six months. After that, we do a few scans once a year, then we just see patients based on symptoms, and they also follow up with our long-term clinic.
What advice do you have for families and caregivers who are facing this diagnosis?
Here at NewYork-Presbyterian, we have a very robust team with doctors and neuro-oncologists, neurosurgeons, radiation oncologists, neuro-radiologists, social workers, child life specialists, integrated medicine, and school liaisons. We have a lot of resources, and we work together very closely.
The patients and families are never alone with this disease. It’s a hard road to walk, but they don’t have to do it by themselves.

