A New Approach for Treating Glioblastoma
A neurosurgeon explains how a new device could transform treatment for patients with glioblastoma and other malignant brain cancers.
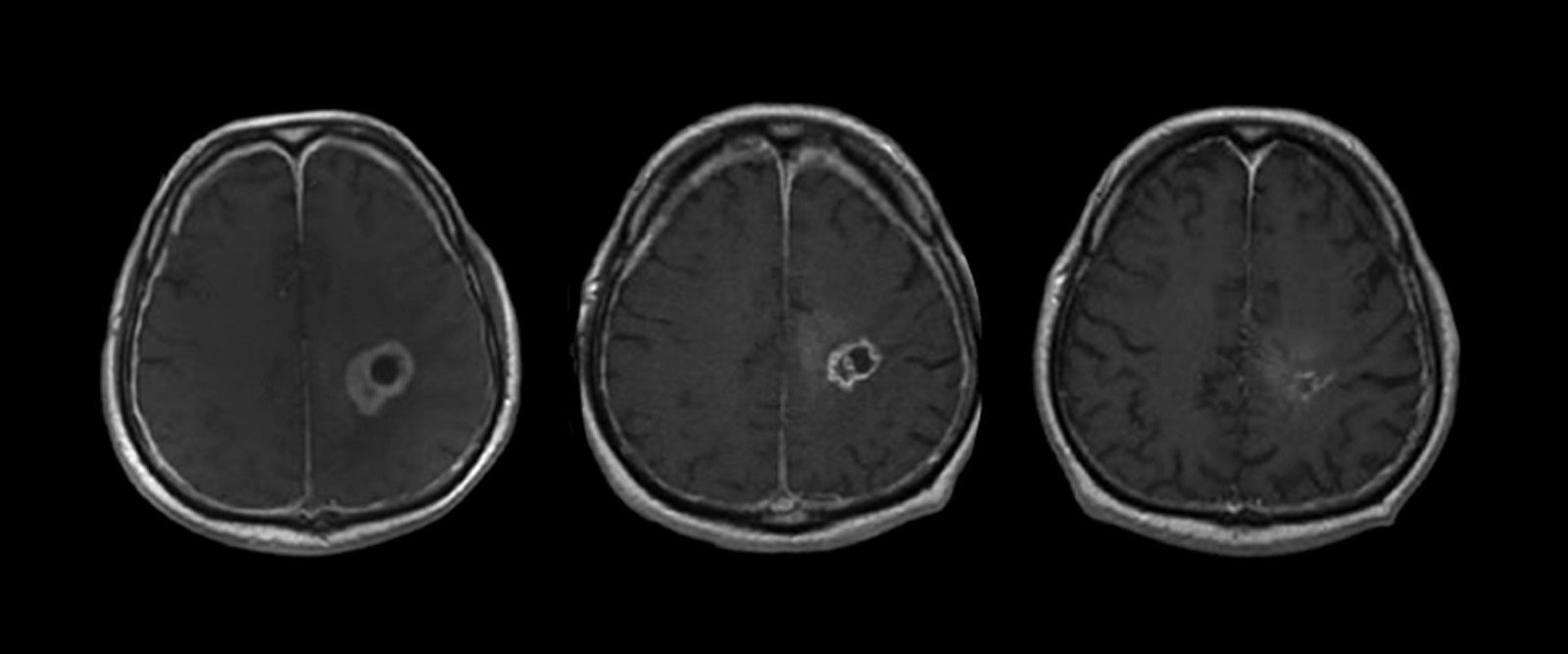
Glioblastoma tumor shrinks after drugs are delivered directly into the brain.
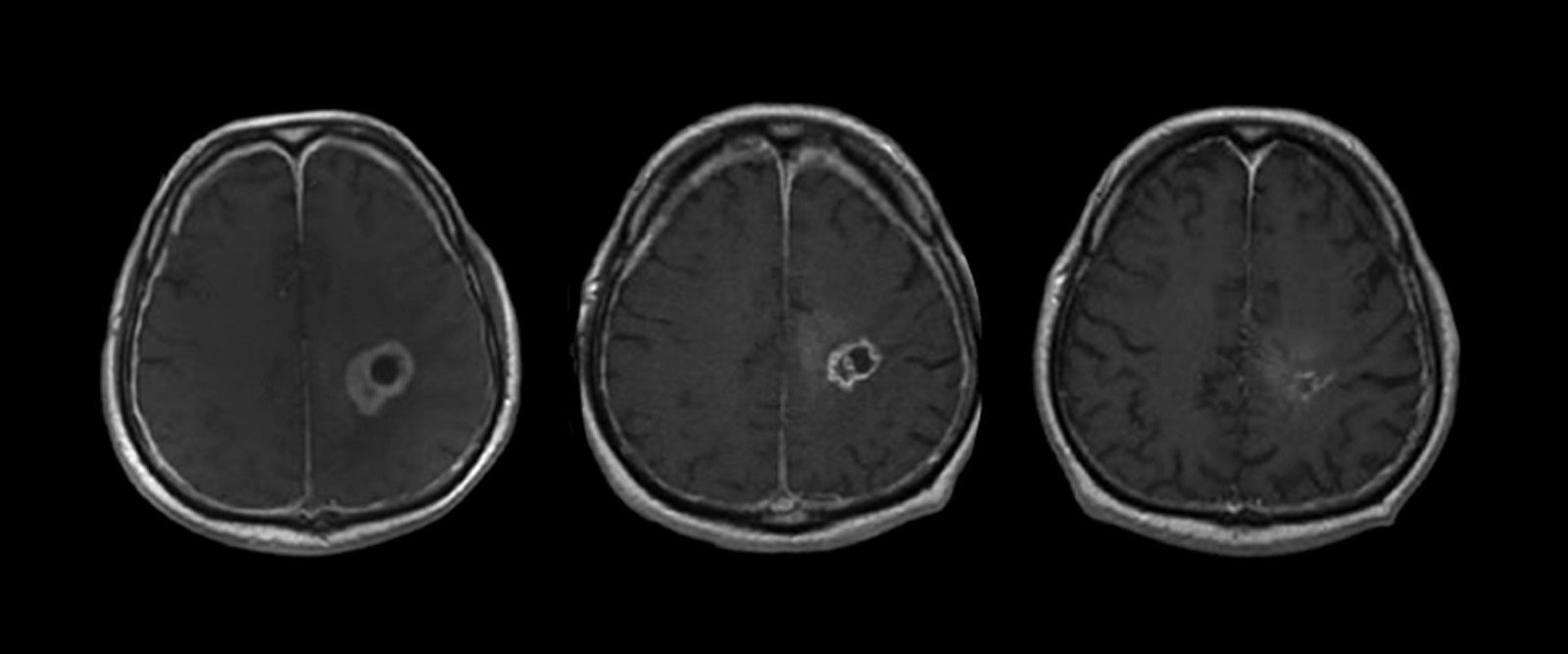
Glioblastoma tumor shrinks after drugs are delivered directly into the brain.
Glioblastoma is the most common type of malignant brain tumor, with approximately 15,000 new diagnoses a year. Patients are typically first treated with surgery to remove as much of the cancer as possible, followed by radiation and chemotherapy.
“Median survival for patients who undergo treatment for glioblastoma is around 12 to 15 months. Usually the tumors return, and once that happens the prognosis is usually only around four or five months,” says Dr. Jeffrey Bruce, a neurosurgeon at NewYork-Presbyterian/Columbia University Irving Medical Center.
While there is no cure for glioblastoma, Dr. Bruce and his team have developed an innovative approach for treating the cancer: a fully implantable pump that continuously delivers chemotherapy through a tube directly into the brain. A recent study in Lancet Oncology found that the device effectively kills brain tumor cells and offers a safe way to treat patients with brain cancer.

Dr. Jeffrey Bruce
“This new approach has the potential to transform treatment for patients with brain cancer with the hope of improving outcomes where the outlook for survival remains very poor,” says Dr. Bruce.
For Glioblastoma Awareness Day, Health Matters spoke to Dr. Bruce, who is also director of the Bartoli Brain Tumor Research Laboratory at Columbia University Vagelos College of Physicians and Surgeons, to learn more about this new approach to treating glioblastoma and what it may mean for patients living with this devastating illness.
Why is brain cancer so resistant to treatment?
Dr. Bruce: We have a lot of good medications to treat brain cancer. But a natural defense mechanism in our body called the blood-brain barrier makes it hard to deliver medicine directly to the brain. The blood-brain barrier is important to keep poisons, viruses, and bacteria found in the blood from getting into the brain, but it also blocks medications from getting into the brain. The problem isn’t killing the brain tumor, the problem is the drug delivery system.
In theory, doctors could give patients higher doses of chemotherapy — via pills or intravenously — to overcome the blood-brain barrier and get more chemo into the brain. But at higher doses, the medications cause too many side effects in other parts of the body, and patients generally cannot tolerate them. As a result, the amount of chemotherapy that can be given safely to patients with brain tumors is invariably ineffective.
Is there a way around the blood-brain barrier?
Over the last decade, my team and I have been working on a pressurized pump to bypass the blood-brain barrier and direct chemotherapy to the area of the brain where the tumor is located.
How does this work?
A small pump is surgically implanted into the abdomen and connected to a thin, flexible catheter threaded under the skin. Detailed imaging guides the surgical placement of a catheter precisely in the area of the brain where the tumor and any residual cancer cells are located.
Once in place, the drug is pumped very slowly, literally at several drops an hour, allowing it to penetrate into the brain tissue. The drug concentration that ends up in the brain is a thousandfold greater than anything you are likely to get with intravenous or oral delivery.
What happens when the medication runs out?
The pump can be refilled or emptied with a syringe and needle. Wireless technology is used to turn the pump on and off and control the flow rate, ensuring that the medicine seeps in slowly and saturates the tumor without leaking out around the catheter.
With this pump we can give higher doses of chemotherapy directly to the brain without causing the side effects that we get with oral or intravenous chemotherapy. Similar implantable pumps already exist to deliver pain medication to the spinal cord and can remain in place for years.
How well does the pump for brain cancer work in terms of treatment?
Though the number of patients in our study was too small to detect an overall survival benefit, an analysis of pretreatment and posttreatment biopsies showed that the chemotherapy was working: The number of actively dividing tumor cells decreased significantly, whereas normal brain cells were not affected.
The five patients who were part of the clinical trial had four treatments over the course of one month. During that time the patients went about their normal routines at home while treatment continued, drip by drip. The patients were walking, talking, eating — doing all of their normal daily activities. They wouldn’t even know whether the pump was on or not.
Could this new approach of medication delivery cure brain cancers like glioblastoma?
While there is still no cure for glioblastoma, getting medication directly into the brain can slow down the growth of the cancer, potentially prolonging people’s lives. Based on the clinical trial data, the results are promising that using this new method of medication delivery could offer patients the hope of a safe and effective treatment for glioblastoma.
The study was conducted in people with recurrent glioblastoma. Would this pump also work in newly diagnosed people?
New studies are being planned to determine if the treatment is also safe for patients with newly diagnosed glioblastoma and if it can improve survival. This approach would give us the ability to change the treatment over time and consider using other types of chemotherapy that would not be effective if given orally or intravenously, but may be much more effective when delivered directly to the brain.
Can this device be used to treat other diseases that affect the brain?
While more studies are needed to better understand how effective this new approach is, using a pump to bypass the blood-brain barrier could potentially be used to treat any brain disease that relies on drug delivery, such as Alzheimer’s, Parkinson’s, or epilepsy.
-A version of this article first appeared on Columbia University Irving Medical Center’s newsroom.
Jeffrey Bruce, M.D., is a neurosurgeon at NewYork-Presbyterian/Columbia University Irving Medical Center, director of the Bartoli Brain Tumor Research Laboratory at Columbia University Vagelos College of Physicians and Surgeons, and co-director of the William Rhodes and Louise Tilzer-Rhodes Center for Glioblastoma at NewYork-Presbyterian. He is a leading authority on complex tumors of the brain and skull base, specializing in the surgical treatment of gliomas, meningiomas, pituitary tumors, skull base tumors, craniopharyngiomas, and pineal tumors. His surgical expertise includes extensive experience with minimally invasive techniques and stereotactic surgery as well as surgical alternatives such as radiosurgery.
Additional Resources
To learn more about the neuroscience services at NewYork-Presbyterian, please visit www.nyp.org/neuro.

