Living With Endometriosis: A 12-Year Journey
After more than a decade of living with chronic pain and heavy periods, a patient finally gets relief from her endometriosis with the right treatment plan.

For 12 years, Crystal Richardson went from doctor to doctor to understand what was causing the debilitating period pain she had been living with since her late 20s. “I had very sharp pains during my period. It felt like my whole pelvic region was being squeezed,” says Crystal, who is now 40 and lives in Brooklyn with her 19-year-old daughter and partner. “It was excruciating.”
Over the years, Crystal’s pain became chronic, with it worsening during each menstrual cycle. It was not uncommon for Crystal to visit the emergency room for cortisone shots and pain medicine to ease the clenching feeling and tightness during her periods. Her menstrual flow was so heavy that she was anemic, making her feel fatigued, dizzy, and light-headed.
The pain got so bad that she had to leave her job because she couldn’t get out of bed during her periods. Daily activities — grocery shopping and errands — also had to take a backseat. “I felt like I was just stuck with these symptoms for the rest of my life,” she says.
Crystal’s exhausting search for answers left her almost hopeless. Finally, Crystal made an appointment with Dr. Eung-Mi Lee, a gynecologic surgeon at NewYork-Presbyterian Lower Manhattan Hospital and the Endometriosis and Pelvic Pain Program at Weill Cornell Medicine.
“When I first saw Crystal, it was clear she was in a lot of pain,” says Dr. Lee. She recalls one visit in which Crystal came into the clinic crying and unable to stand without help. “What struck me about her case was that it had a huge impact on her quality of life in a way that made it hard for her to work and carry out normal activities,” she says.
A Delayed Diagnosis
After her visit with Dr. Lee in September 2023, Crystal soon learned that she had endometriosis, in which tissue similar to the lining of the uterus, called the endometrium, grows outside the uterus. Crystal’s symptoms were classic for the disease. Endometriosis also can cause difficulty getting pregnant, inflammation, and scarring, and affect nearby organs like the appendix, bladder, and bowel if it spreads.
Compounding her pain, Crystal also had adenomyosis, which Dr. Lee describes as “a cousin to endometriosis.” With endometriosis, the endometrial-like tissue finds its way outside of the uterus, like the ovaries and fallopian tubes, while with adenomyosis the tissue grows into the muscle of the uterus.
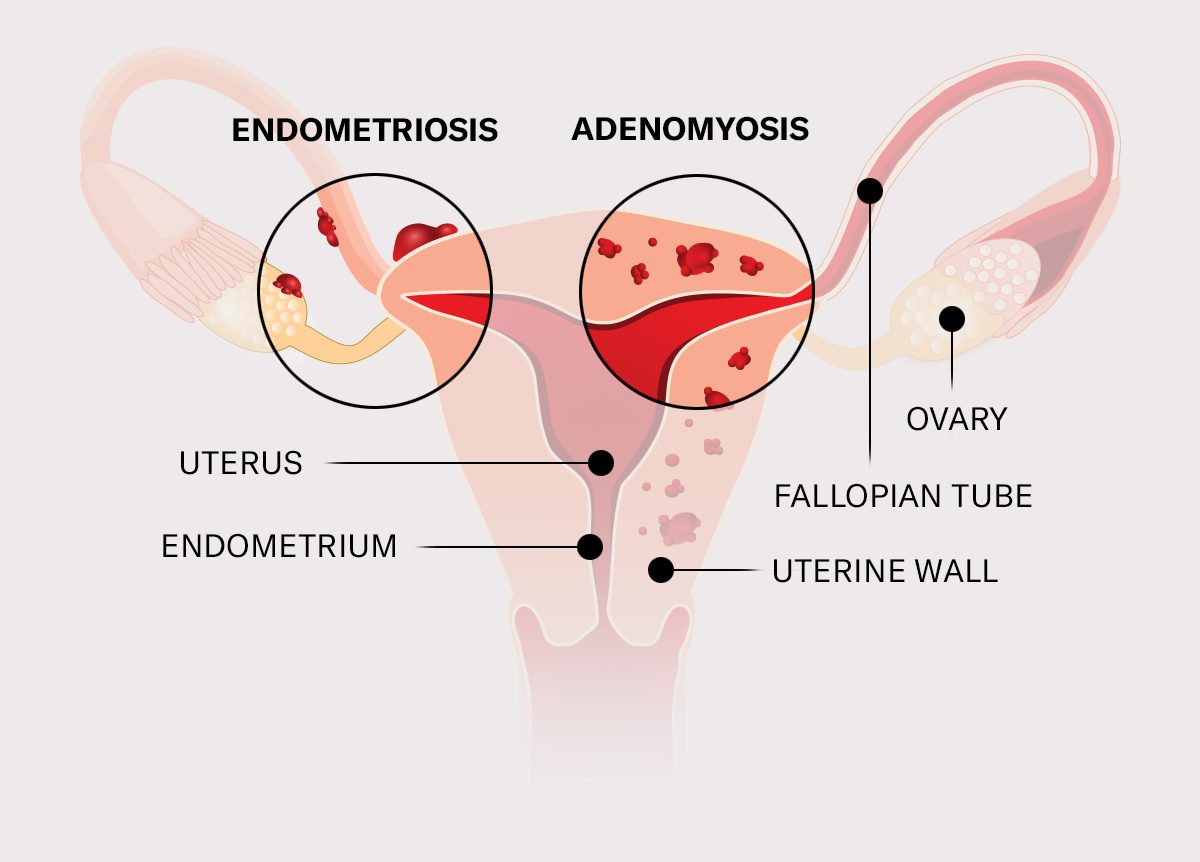
Similar to endometriosis, adenomyosis can cause painful and heavy periods, pelvic pain, pain during sex, and a feeling of fullness or bloating. It can also cause the uterus to enlarge.
Over the years, Crystal saw numerous doctors who had explored her symptoms. Some suspected endometriosis and performed ultrasounds. “I was told, ‘we didn’t find anything,’” Crystal says. “I was even getting, ‘maybe it could be in your mind.’”
Delayed diagnosis with endometriosis is not uncommon, says Dr. Lee. Recent research shows that endometriosis is characterized by delays of up to 11 years from the onset of symptoms to a diagnosis.
Dr. Lee explains that while ultrasounds are helpful and rule out other conditions, “It can’t tell us whether or not people have endometriosis,” she says. “I hear patients say, ‘I got an ultrasound and it looked normal so I was told I didn’t have endometriosis.’ Unfortunately, there are no great screening tools, and confirmation of the disease is made by surgery.”
Another challenge is that endometriosis symptoms are not specific only to the disease. People can have these symptoms for other reasons such as uterine fibroids, ovarian cysts, or a gastrointestinal issue.
Indeed, Crystal had other issues, including diverticulosis and fibroids. In 2017 she underwent a procedure called fibroid embolization to remove her fibroids, which helped relieve her symptoms for a time. But the pain came back.
Dr. Lee sees many patients who have lived with endometriosis pain for years. “I have a lot of patients who say, ‘Well, my mom always had bad periods, and she told me this is just the way it is,’” explains Dr. Lee. “A lot of this pain gets normalized. Unfortunately, this leads many to deal with the pain in silence.”

The Road to Treatment
Dr. Lee took Crystal’s detailed medical history and performed a pelvic exam and ultrasound as the first steps toward a diagnosis. Crystal also had a magnetic resonance imaging (MRI), which showed adenomyosis and enabled Dr. Lee to see if Crystal’s nearby organs were affected by her condition, a helpful tool for planning Crystal’s surgery.
Treatment ultimately depends on each individual’s case. For mild endometriosis and adenomyosis, non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help manage pain, and hormonal therapy can help control bleeding and reduce pain. Over the years, Crystal was put on birth control pills and pain relievers but never found relief.
For those who do not find relief with medical therapy, laparoscopic surgery is a good next step, says Dr. Lee.
Because Crystal wanted to be finished with her periods and her adenomyosis was significant, she chose a hysterectomy. Crystal was not interested in having more children, so this worked for her. But it’s important to note that a hysterectomy for endometriosis or adenomyosis is typically reserved for cases in which other treatments have failed, says Dr. Lee. There are fertility-sparing options for those who wish to become pregnant one day. “Most of my patients choose fertility-sparing options,” says Dr. Lee.
In November 2023, Dr. Lee performed Crystal’s hysterectomy — removing her uterus, cervix, and fallopian tubes. This was done via laparoscopy, a minimally invasive surgery in which small incisions are made in the belly and a tiny camera is inserted to guide the procedure. Laparoscopy is also the gold standard for a definitive endometriosis diagnosis, enabling tissue to be removed for testing.
During the surgery, Dr. Lee saw that Crystal’s endometriosis lined the surfaces inside her pelvis, and that her adenomyosis was so advanced that “she had a very enlarged and rounded uterus the shape of a grapefruit — which is not typical in a normal uterus. She also had a lot of scarring, likely from the combination of endometriosis, adenomyosis, and her previous cesarean section.”
“I could see as soon as we went in for surgery,” says Dr. Lee, “why this would have the impact that it would.”
Living Life Without Pain
Today, Crystal’s pain is almost completely gone. She no longer wakes up with anxiety about her pain. She feels good enough to take daily walks, hit the gym, and run errands — activities she was unable to do before. She now works as a school lunch helper and is excited to get back into hobbies like cycling, an old passion of hers.
“I remember seeing her after surgery, and what a huge difference it seemed to make for her and her level of pain,” says Dr. Lee. “She looks very happy, very hopeful, and she just has so much energy.”
Dr. Lee stresses that if anyone is experiencing very heavy periods, bad menstrual cramps, or painful intercourse, they should see an endometriosis specialist.
Crystal agrees. She tells her friends with painful periods to make sure they get the treatment they need. “Don’t wait until the pain is debilitating,” says Crystal. “I want people to know that there is help out there. Dr. Lee gave me my life back. I’m sharing my story so that others can get the help they need and not feel so alone.”
Additional Resources
Learn more about NewYork-Presbyterian’s services for endometriosis.
Eung-Mi Lee, M.D., is a board-certified obstetrician-gynecologist with advanced specialist training in Minimally Invasive Gynecologic Surgery (MIGS) with NewYork-Presbyterian/Weill Cornell Medical Center, NewYork-Presbyterian Lower Manhattan Hospital, and the Endometriosis and Pelvic Pain Program at Weill Cornell Medicine. She is an assistant professor of clinical obstetrics & gynecology at Weill Cornell Medicine. Dr. Lee cares for patients with endometriosis, adenomyosis, fibroids, ovarian cysts, and more.
