Is It Seasonal Allergies or COVID-19?
The start of spring also means the beginning of seasonal allergies. Here’s how symptoms of allergies differ from warning signs of COVID-19.

As the weather changes and the trees begin to spread their pollen, you may be wondering whether your respiratory symptoms are caused by allergies – or something more serious? Dr. William Reisacher, an associate attending otolaryngologist at NewYork-Presbyterian/Weill Cornell Medical Center and Professor and Director of allergy services in the Department of Otolaryngology – Head and Neck Surgery at Weill Cornell Medicine, explains how to identify the warning signs of COVID-19 that may be a reason to give your doctor a call.
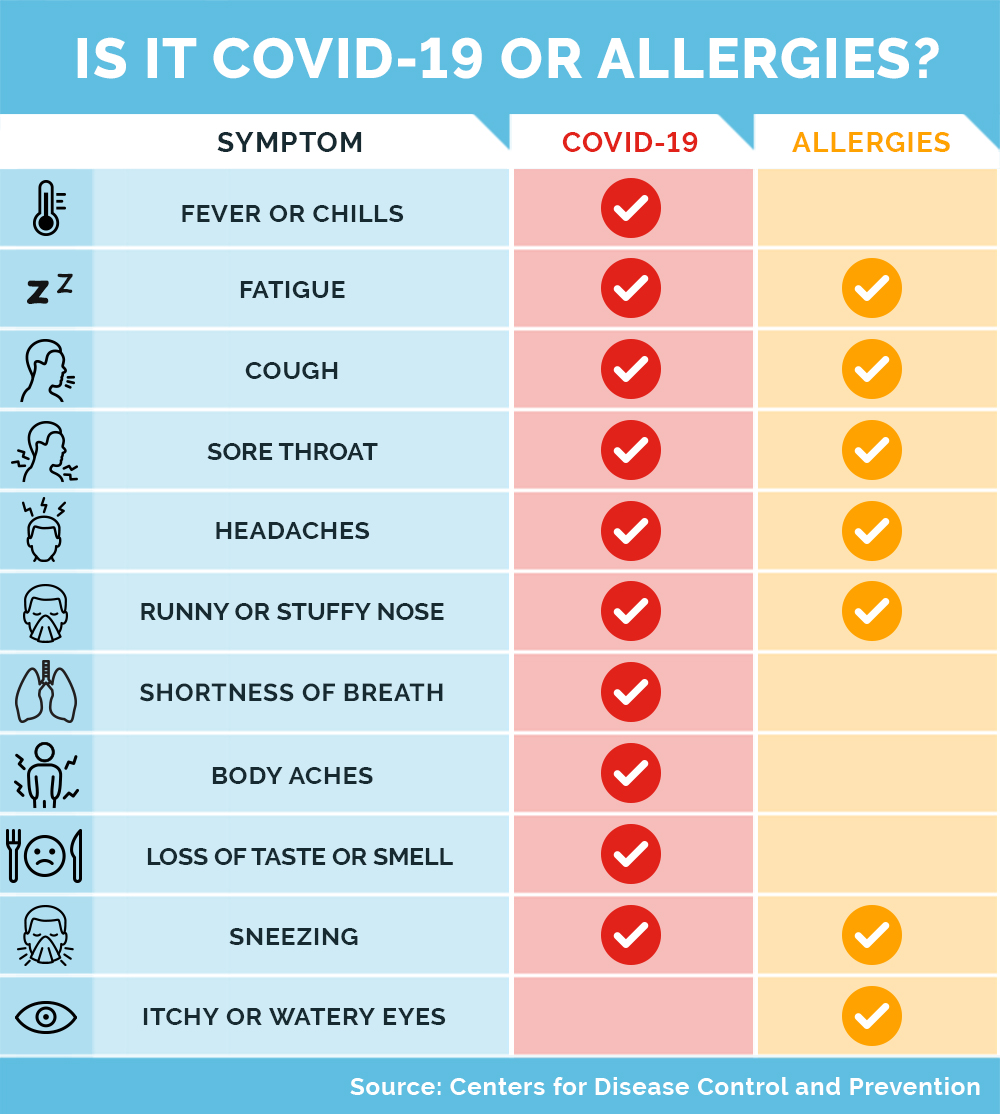
How do the symptoms of COVID-19 differ from the symptoms of spring allergies?
With a viral illness like COVID-19, there is typically a fever, which is not present with allergies. Allergies to pollen cause sneezing and itchiness in the eyes, nose, and throat, which is less common with COVID-19. Cough is a common symptom of COVID-19, which can also be present in some patients with allergies. Sudden loss of smell or taste, without significant nasal symptoms, also points to COVID-19.
Here’s another difference between COVID-19 and seasonal allergies: With seasonal allergies, the symptoms tend to wax and wane and get worse when you are outside. With a viral infection, there’s typically a steady worsening.
Do the symptoms of allergies and COVID-19 express themselves differently in children than in adults?
Kids with allergies tend to be restless, while adults who have allergies are more fatigued. If a child is lethargic and feverish and has a persistent cough, with or without itchy eyes and a runny nose, then the pediatrician should be notified.
Are people with allergies more susceptible to coronavirus than others are?
At this point, there is no evidence that people with allergies to pollen are more susceptible to COVID-19. While people with compromised immune systems are at higher risk of severe COVID-19, people with allergies don’t have a compromised immune system; their allergies are actually an overreaction of the immune system.
That said, among people with some degree of asthma, those with worse disease tend to be in a higher-risk group for viral infections, particularly if the asthma is not well managed. So this is a good time to review the way you are managing your allergies – and your asthma, if you have it. You and your doctor can go over the ways you are managing your condition and make any modifications if needed.
Should we be worried about inhalers inadvertently spreading the virus by turning airborne droplets into a finer aerosol?
With any viral infection, doctors have to pay attention to the risk of aerosolization. But inhalers can be used safely by a patient, and they should be used when they are needed, whether you are at home or outside. If you have to use inhalers, however, it’s still very important to give extra distance when around other people.
A lot of people are using this time spent at home to spring clean. Any tips for those with spring allergies?
If your allergy is due to pollen, being inside may be helpful, and if spring cleaning makes you feel better, that’s a benefit. Do keep in mind that cleaning can kick up a lot of dust, so if you are allergic to indoor allergens, make sure to have adequate ventilation and keep that mask handy.
Can someone who has other kinds of severe allergies, such as an allergy to nuts or animals or to a plant, get the COVID-19 vaccine?
Allergies to airborne items, such as pollen, dust and pet dander, or food allergies do not disqualify you from getting the COVID-19 vaccine, even if you are receiving allergy immunotherapy. It is important to discuss with your allergist, however, on whether you should hold off on treatment around the day of the vaccine. Very mild reactions to the first vaccine also do not disqualify you from receiving the second, but more serious reactions should be discussed with your physician.
This story first appeared on Weill Cornell Medicine’s patient-care blog.
