Making Endoscopic Surgery More Effective
A NewYork-Presbyterian doctor creates a new gastrointestinal application that eases use for physicians and improves patient care.
Dr. Jeff Milsom compares performing procedures in the intestinal tract with an endoscope to rowing a boat in moving waters: The intestine, like the water, is not stagnant. While it’s possible to do simple things while the water or the intestine is bobbing up and down, more complex movements are impossible.
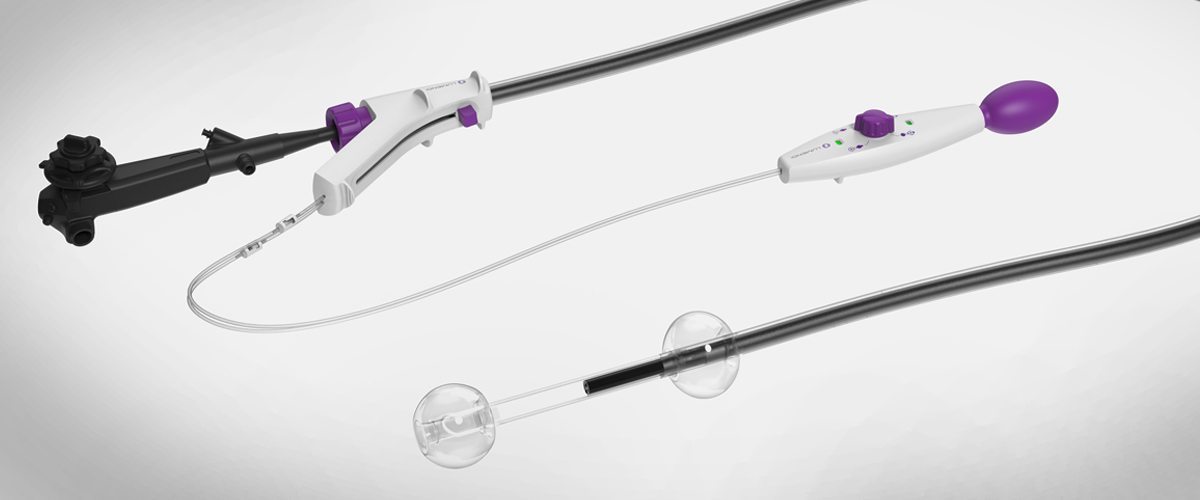
To alleviate that, Dr. Milsom, chief of colon and rectal surgery at NewYork-Presbyterian/Weill Cornell Medical Center, created an “anchor” called the DiLumen, a sleeve that slides onto a traditional endoscope. The innovative instrument has a balloon on each end of the scope that inflates, creating a closed zone that straightens out and steadies the intestine, giving doctors a clear and steady picture of the diseased area.
“The effect of creating that zone allows a doctor to see and treat a given lesion more confidently,” Dr. Milsom says.
The tool was born out of a collaboration among surgeons, imaging specialists, engineers, and clinicians in the Minimally Invasive New Technologies (MINT) program at NewYork-Presbyterian and Weill Cornell Medicine. In 2014, industry partner Lumendi licensed the technology.
As clinical trials get underway – they begin at NewYork-Presbyterian in April — the DiLumen will, Dr. Milsom believes, change how digestive diseases are treated. Lesions are often situated around a bend in the intestine or hidden behind a fold, making it difficult for doctors using traditional endoscopes to see well enough to address the problem. The DiLumen straightens the area of the intestine between the two balloons, improving visualization and increasing the odds problems like benign polyps, strictures, diverticulitis, and inflammatory bowel diseases can be treated with a scope, not surgeries.
“There are tens of thousands of patients per year who, in the United States, undergo major colon surgeries simply because the doctor with a colonoscope can’t really see the lesion well enough, or long enough, to adequately treat it that way,” Dr. Milsom says.
Unlike conventional intestinal surgeries that usually require cutting out a piece of the intestine, this minimally invasive approach eliminates the need for incisions or general anesthetic, increasing patient safety and decreasing hospital stays.

Dr. Jeff Milsom
“We have the capability now, in the intestine, to directly put a high-definition camera inside, and really do surgery inside,” Dr. Milsom says. “This is a world that I believe that we can pioneer.”
Research shows that open gastrointestinal surgeries have average hospital stays of eight days and laparoscopic procedures have average hospital stays of five days. In comparison, Dr. Milsom estimates that the average hospital stays for procedures performed with the DiLumen will be just one to two days.
Costs will be dramatically lower, too, thanks to less need for anesthesia and shorter hospital stays.
The U.S. Food and Drug Administration approved the DiLumen in December 2016.
Dr. Milsom is already working on a pipeline of complementary products, including the DiLumen C2, a tool with two extra instrument channels for tools that can grasp or cut tissue, coagulate blood vessels, and suture and close wounds. Adding these channels to the DiLumen will make it possible to perform more complex procedures.
All of the technology, Dr. Milsom explains, was created to achieve a singular goal: To drive innovation in healthcare.
“We want to improve patient care, to make medicine better and less expensive,” he says. “With this approach we have a chance to really open up a whole new avenue of therapies for digestive disorders.”
