What to Know Before Your Next Mammogram
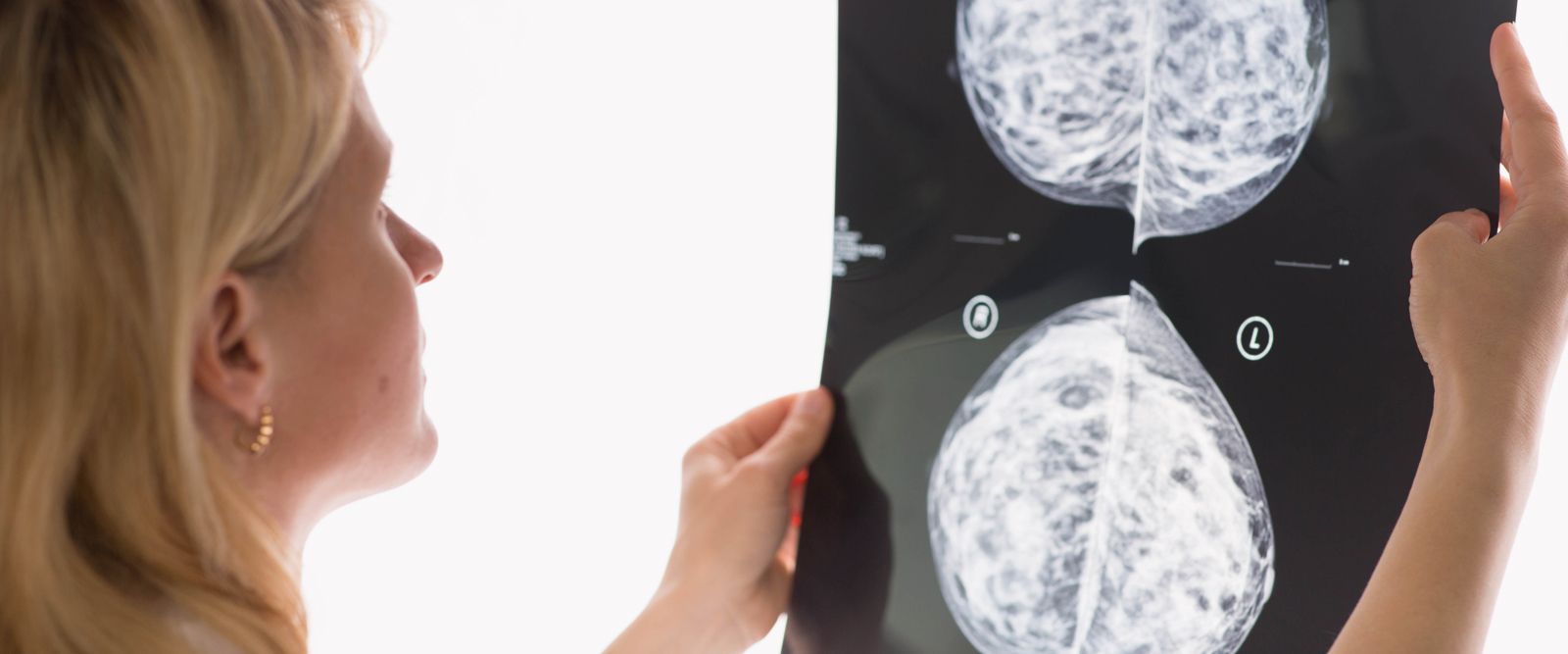
A radiologist explains why getting a routine mammogram starting at age 40 is important and how best to prepare.
If you don’t feel prepared for your first mammogram, or you’re anxious about your annual visit to the radiologist, you’re not alone. According to the Centers for Disease Control and Prevention, only about 65% of women ages 50-74 are up to date with their mammograms.
However, the U.S. Preventive Services Task Force recently updated their guidelines to recommend that women start getting mammograms at age 40. The American College of Radiology and Society of Breast Imaging also recommend that women of average risk get annual mammograms beginning at age 40.
Here, Dr. Elizabeth Kagan Arleo, an attending radiologist at NewYork-Presbyterian/Weill Cornell Medical Center and a professor of radiology at Weill Cornell Medicine, discusses what people need to know about the screening and why it’s important to make your annual visit.
1. It’s normal to feel nervous about a mammogram, but you should still go.
“The whole experience can be anxiety-provoking — before, during, and after. It can be helpful to acknowledge that, and then move on to focus on why do it in the first place. And that’s because annual screening mammography, starting at age 40, prevents the most deaths from breast cancer.” A study published in the journal Cancer in August 2017 and co-authored by Dr. Arleo, found that the greatest reduction in breast cancer-specific mortality is achieved with annual screening starting at 40.
Dr. Arleo adds that the American College of Radiology made new recommendations in 2018 that “all women, especially black women and those of Ashkenazi Jewish descent, should be evaluated for breast cancer risk no later than age 30, so that those at higher risk can be identified and can benefit from supplemental screening.” Women can be evaluated for breast cancer risk by having a conversation with their doctor, including ob-gyns, internal medicine or family medicine physicians, to discuss their family history and any additional known risk factors. If applicable, their doctor may recommend genetic counseling or testing.

Dr. Elizabeth Kagan Arleo
2. Bring your medical history with you for the best care.
“A week to a month before a mammogram, if a woman’s not going to a radiology practice she’s been to before, she should locate her prior images [the actual images, not just the reports] and bring them to the new appointment,” says Dr. Arleo. “Having prior studies for comparison is really important because part of the evaluation is looking not only for masses and calcifications, but also for changes in the breast tissue pattern, and without any prior images, that part is missing. Having prior images can also minimize the need for additional imaging evaluation.”
3. Go au naturel the day of your test.
Don’t wear deodorant to your appointment. “It can appear on the mammogram as little white dots, which can look like calcifications, which in some cases can be the earliest sign of breast cancer,” says Dr. Arleo. Also consider wearing a skirt or pants with a separate top, so when you get undressed you can remove your top without having to remove all your clothes.”
4. Team up with your technologist.
“Tell the mammogram technologist if you have any new lumps and then work with her to get the best possible images,” says Dr. Arleo. The positioning and pressure may be uncomfortable; however, it lasts just a few seconds and enables optimal evaluation of the breasts. As much as possible, just try to relax the body and work with the technologist. “It’s a team effort to get the best possible images,” she says.
5. With annual screening mammograms, don’t let concerns about radiation dissuade you.
“A mammogram is an extremely low dose X-ray, and the risk of the minimal radiation exposure is far outweighed by the potential mortality benefit,” says Dr. Arleo.
6. Family history counts.
“Women at high risk of breast cancer, defined mainly on the basis of a genetic mutation or family history, should start annual screening earlier,” says Dr. Arleo. “For example, if your mother or sister was diagnosed with breast cancer at 46, then you should start getting annual mammograms at 36 years old.”
7. You still need a mammogram, even with no family history.
Even if you don’t have a family history or other risk factors, this doesn’t mean that you shouldn’t get screened, says Dr. Arleo. “The fact of the matter is that 60 to 70 percent of women diagnosed with breast cancer have no known risk factors,” she says.
8. Annual screening mammography saves lives.
On your way out, book for next year to ensure that you actually get annual screening mammography. “If you haven’t had a mammogram in the last year, then call your healthcare provider so they can help you to do so,” says Dr. Arleo.
