Your Pregnancy: A Guide to Prenatal Genetic Testing
Genetic tests can help you plan for pregnancy and birth.
Pregnancy is a time of joy and excitement. But it’s natural to be concerned about your baby’s health.
Prenatal genetic tests can provide parents with important information about their baby during pregnancy to help them make the best health decisions and get expert care, says Dr. Emilie Vander Haar, associate director of OB Ultrasound and Prenatal Testing at NewYork-Presbyterian Alexandra Cohen Hospital for Women and Newborns. Here are some of the most common tests you may be offered before and during pregnancy.
Carrier Screening Before Conception
A carrier of a genetic disorder has one normal gene and one mutated gene in a specific gene pair. If both parents are carriers, their child can have the genetic condition.
“If you have a strong family history of or a prior pregnancy affected by a genetic condition, you might want to meet with a genetic counselor before conceiving,” says Dr. Vander Haar, also an assistant professor of obstetrics and gynecology at Weill Cornell Medicine.
The work-up involves taking blood samples to look for inherited conditions, such as Tay-Sachs disease or cystic fibrosis, that parents might pass to their children. “If you’re thinking ahead to pregnancy, you and your partner can both get tested to make sure that you don’t carry the same mutation,” says Dr. Vander Haar.
If couples do carry the same mutation, they can discuss with a genetic counselor the chance that their baby will be affected as well as other tests and options to consider.

Dr. Emilie Vander Haar
Genetic Screening Tests
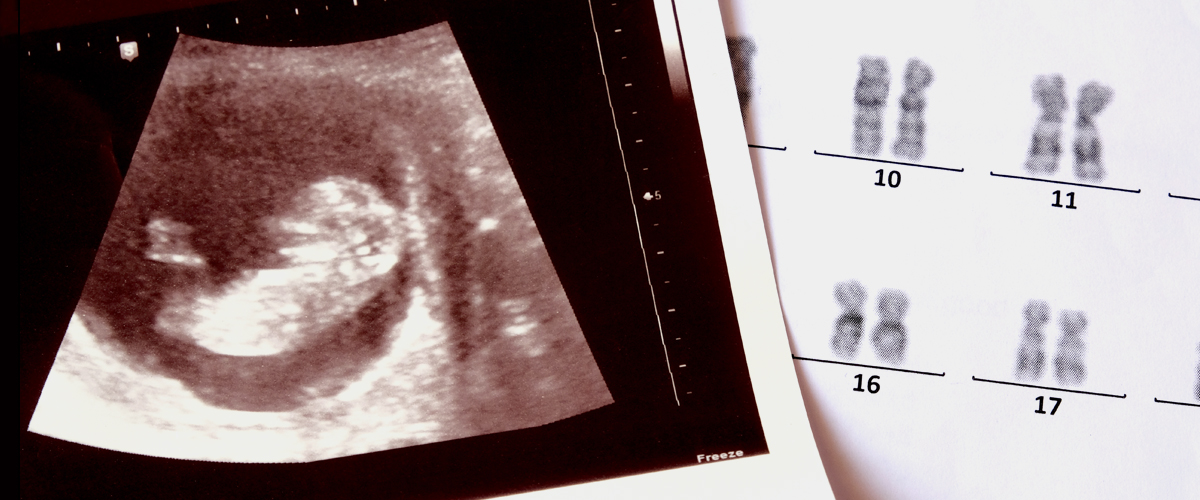
During pregnancy, the first step is prenatal screening. These tests calculate the risk of having a child with a genetic condition and are performed as early as the 10th week of pregnancy.
Prenatal screening is offered with every pregnancy, but it is particularly important for those over age 35. Moms-to-be usually receive one of these tests:
The first trimester screening
This includes a blood test that measures two pregnancy-specific substances (known as serum analytes) in the blood; abnormal levels are linked to genetic disorders. It also includes a nuchal translucency test, which uses an ultrasound exam to measure the thickness of the clear space at the back of the unborn baby’s neck. The screening is done between 11 and 14 weeks of pregnancy.
Results are compared to those of other mothers to come up with a risk score for estimating whether a baby will be affected, says Dr. Vander Haar.
“If the risk is one in 10,000, that means the likelihood of having an abnormality is really low,” says Dr. Vander Haar. “If it’s one in 200, that’s high enough that we would recommend that you consider further testing.”
The screening is very good at assessing risk for Down syndrome and other genetic conditions, such as trisomy 13 and trisomy 18, says Dr. Vander Haar. Babies with these conditions have an extra chromosome, which results in intellectual disabilities and birth defects.
The second trimester screening
Patients who miss the window for the first trimester screening for these conditions may get a second trimester screening, a blood test also known as the quad screen because it measures four serum analytes. It’s performed between 16 and 20 weeks of pregnancy.
Some doctors perform both first and second trimester screenings and combine the results to determine an overall risk. “This combined screening can be more accurate than either screening alone, but you won’t receive results until after the second trimester test is done,” says Dr. Vander Haar.
Cell-free fetal DNA screening
Cell-free fetal DNA is a newer test that examines fetal cells found in a mother’s blood and then reports whether the pregnancy is at low or high risk for genetic conditions. This blood test is exceptionally sensitive for Down syndrome, trisomy 13, and trisomy 18.
“Overall in women over 35, it seems to have 98% to 99% accuracy,” says Dr. Vander Haar. “That means, if you have a negative result, it’s a true negative result.”
Sometimes the results of the screening aren’t positive or negative, however. In this case, “you might need a repeat blood sample, or we might move to CVS or amniocentesis,” says Dr. Vander Haar.
“If a screening test is positive,” adds Dr. Vander Haar, “there is a chance that it is a false positive, and thus we would always recommend diagnostic testing in these cases.”
Diagnostic Tests: Chorionic Villus Sampling (CVS) and Amniocentesis
If a screening test indicates a high risk for having a child with a genetic condition, your doctor will likely recommend a diagnostic test to confirm or rule out a diagnosis. These tests also pick up more potential genetic abnormalities than screening tests, says Dr. Vander Haar. But they carry a very small risk of miscarriage.
Chorionic villus sampling (CVS)
With CVS, the doctor inserts a specialized catheter through the cervix or a long needle through the abdomen and collects cells from the placenta. This test is typically done between weeks 11 and 14 of pregnancy.
Amniocentesis
During amniocentesis, a needle is inserted through the mother’s abdomen into the uterus to take a sample of amniotic fluid. This test is performed between weeks 15 and 20 of pregnancy.
Either one is a reasonable option,” says Dr. Vander Haar. “But sometimes you don’t have the results of genetic screening back before the window for CVS closes. Then your option is amniocentesis.”
Be aware that diagnostic tests can also be inconclusive. For instance, they may show a mutation in a gene that hasn’t been linked to a disorder yet or point to a known condition but not indicate how severe it will be.
“That can be tricky for parents,” says Dr. Vander Haar. “There are just some things that we still don’t know.”
Ultrasound
Ultrasound, which uses sound waves to capture images from inside of the body, is an important tool for detecting genetic conditions. “We do a full anatomical survey of the fetus around 18 to 20 weeks,” says Dr. Vander Haar. “If there is an anatomic abnormality, there’s usually a higher likelihood of a genetic abnormality, and we might encourage someone toward amniocentesis if they haven’t had a diagnostic test yet.”
For instance, an unborn baby’s heart problem could be a sign of DiGeorge syndrome, a genetic condition that causes heart defects, developmental delays, and problems with the immune system. It can only be picked up with CVS or amniocentesis, says Dr. Vander Haar.
Getting the Right Care
Not every parent-to-be chooses genetic testing. Some couples want to deal with situations as they come.
Yet, “there are other patients who say, ‘I want to know if my baby has Down syndrome. I want to plan ahead,’” says Dr. Vander Haar.
If parents choose genetic testing and the baby has a serious condition, Dr. Vander Haar recommends the following:
- Seek care from a maternal-fetal medicine specialist, a doctor who is trained to manage high-risk pregnancies.
- Consult with a pediatrician who specializes in the type of care your child will need, such as a pediatric neurologist or cardiologist.
- Connect with organizations like March of Dimes or the National Down Syndrome Society for information and support, or look for a local parents’ support group.
- Plan to give birth in a hospital that has an advanced neonatal intensive care unit (NICU). Says Dr. Vander Haar, “If there are anatomic abnormalities associated with the genetic condition, you’re going to want to deliver where you can get high-level NICU care as well as pediatric surgery.”
Emilie Vander Haar, M.D., is an ob-gyn, maternal-fetal medicine specialist, and associate director of OB Ultrasound and Prenatal Testing at NewYork-Presbyterian Alexandra Cohen Hospital for Women and Newborns, with expertise in high-risk obstetrics. She is also an assistant professor of obstetrics and gynecology at Weill Cornell Medicine. Dr. Vander Haar specializes in obstetric ultrasound and prenatal diagnostic procedures.
