Your Guide to Pelvic Floor Disorders
An expert explains what to know about the pelvic floor, including symptoms of and treatments for conditions such as incontinence and prolapse.

Pelvic floor disorders, such as incontinence, painful sex, and pelvic organ prolapse, are common conditions that many women and gender-nonconforming people struggle with. In fact, one in four women have reported having had at least one pelvic floor disorder and approximately half of American women will experience urinary incontinence at some point in their lives.
Unfortunately, some patients may be hesitant to speak up about their symptoms, which means they could miss out on effective treatments that could help improve their quality of life, says Dr. Larissa V. Rodríguez, urologist-in-chief at NewYork-Presbyterian/Weill Cornell Medical Center.
“Many people think they are the only ones who suffer from these conditions and are not aware of how common they are,” says Dr. Rodríguez, director of the new Center for Female Pelvic Health at NewYork-Presbyterian/Weill Cornell Medical Center, which provides comprehensive care for patients with pelvic floor disorders. “There are many things that can be done about these symptoms.”
Dr. Rodríguez, who is also chair of the Department of Urology at Weill Cornell Medicine, shares here what you need to know about common pelvic floor conditions, how to prevent them, and the various treatments that are available.

Dr. Larissa V. Rodríguez
What is the pelvic floor?
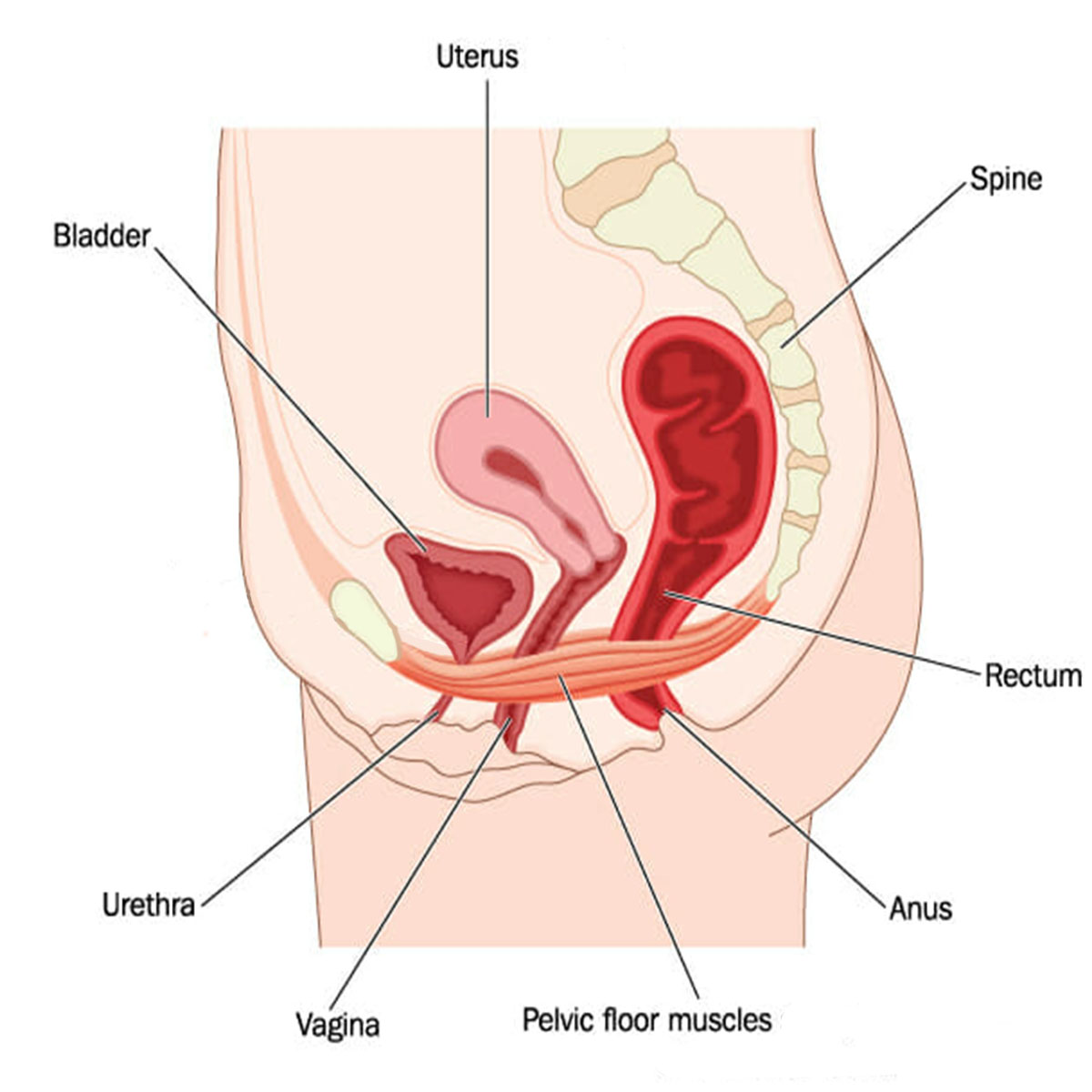
The pelvic floor is a collection of small muscles on the inside of the pelvis. The rectum, the vagina, and the urethra go through those muscles, which is why normal function of those muscles is important for the GI tract, the urinary tract, and sexual and vaginal functions.
What are the common pelvic floor disorders?
Pelvic floor disorders in the urinary tract include urinary incontinence — such as loss of bladder control when laughing, sneezing, or exercising — and other voiding problems or even the inability to urinate. In the vaginal region, disorders include problems with sexual function and pain during intercourse, as well as prolapse, which is when pelvic floor muscles weaken and allow organs to sag and protrude into the vagina. In the rectum, it’s fecal incontinence (the involuntary leakage of stool) or severe constipation.
What are the main causes of pelvic floor disorders?
Vaginal births are one of the biggest risk factors for developing these disorders either immediately after delivery, or, more commonly, later in life, around menopause. We know that declining hormone levels play a role in causing systemic changes in the pelvic floor and atrophy of the vaginal region.
Aging, smoking, and diabetes, in particular, correlate with some of these conditions. Things that increase abdominal pressure, such as a chronic cough and obesity, which put a lot of strain on the pelvic floor, increase the risk for pelvic prolapse and incontinence.
And people can experience painful intercourse after menopause, vaginal surgery, sexual assault, or pelvic trauma of any sort.
Can pelvic floor disorders be prevented?
These disorders can develop over time. A routine pelvic exam or Pap test is a good opportunity for doctors to ask patients about symptoms.
Managing conditions like diabetes and obesity can help prevent pelvic floor problems from worsening. And performing certain exercises, like Kegels, especially around pregnancy, can be preventive and therapeutic.
A Workout for Your Pelvic Floor
You can strengthen your pelvic floor muscles with exercises known as Kegels. The first step is to identify these muscles by imagining that you are trying to keep yourself from passing gas or trying to stop the flow of urine. Then follow these steps:
- Make sure your bladder is empty, and then sit or lie down.
- Tighten your pelvic floor muscles. Hold for three to five seconds.
- Relax the muscles and count three to five seconds.
- Repeat 10 times, three times a day.
How are pelvic floor disorders diagnosed?
Most people can be diagnosed with a physical exam that may include a urinalysis to rule out things like urinary tract infections (UTIs), as recurring UTIs can account for incontinence. In addition, an ultrasound of the bladder can determine whether or not a patient is able to empty it normally.
Occasionally, slightly more advanced diagnostic tests are needed, including urodynamics, which allow us to see what’s happening to the bladder when it fills with urine and when people urinate. We can also see bladder spasms and whether they lead to leakage or a sensation of urgency. Testing also evaluates how efficiently a patient voids.
A cystoscopy allows us to look inside the bladder and ensure there’s not an irritant, such as a rare bladder stone or a tumor, that might be causing urinary symptoms.
Most prolapse cases can be accurately diagnosed with a pelvic exam. Rarely, we may do imaging such as a dynamic MRI to evaluate which organs are dropping and to aid in the diagnosis of fecal incontinence if it is a coexisting symptom.
Treatments for Pelvic Floor Problems
There are a variety of approaches to treating pelvic floor disorders, says Dr. Rodríguez. Choosing one depends on many things, such as the severity of the symptoms and other health problems an individual may have as well as their goals and how active they are. No matter what pelvic floor issues you’re experiencing, it’s best to speak with a pelvic floor specialist to determine which treatment may be right for you.
Pelvic Floor Physical Therapy
A specialized therapist uses exercises and other techniques, such as relaxation and biofeedback, that can help you control your pelvic floor muscles. These techniques can help people with urinary and fecal incontinence, mild prolapse, and painful intercourse.
Behavior Changes
Changing lifestyle habits can improve symptoms. For example, curbing coffee and alcohol intake can reduce incontinence, and eating more high-fiber foods can help bowel movements.
Medications
Medications can improve problems such as incontinence (and they pose few side effects). For example, some prescription medicines help the bladder relax and not spasm so people can hold urine longer.
Nerve Stimulation
Stimulating specific nerves can work to block abnormal signals to the bladder that lead to urinary incontinence. With nerve stimulation, electrodes are placed inside the vagina or other sites on the body to deliver mild electric impulses to treat muscle weakness, spasms, and pain. Nerve stimulation can also be used to help people regain control of bowel function.
Injections
Botulinum toxin (Botox), often used to treat wrinkles, can be quite effective for certain incontinence symptoms. The drug paralyzes muscles in the bladder so that patients don’t have spasms. It can also be used to relax tight vaginal muscles that cause pain during intercourse and to facilitate bowel movements in people with defecation difficulties.
To aid those who leak urine while, say, coughing or jumping, doctors may inject bulking agents into the walls of the urethra to help tighten it so leakage is less likely.
Surgery
For some incontinence cases, sling surgery may be recommended, in which a “sling” made of mesh or human tissue is placed under the urethra to prevent leakage of urine. For prolapse, vaginal surgery or robotic or other minimally invasive procedures may be recommended to lift the pelvic organs back into place.
Are racial disparities a factor in who experiences pelvic floor disorders?
African American women have a higher incidence of overactive bladder (urgent and frequent urination) and urge incontinence (sudden urination and leaking), while stress incontinence (leaking when laughing, coughing, sneezing, or exercising) affects white women at a higher rate. White women also are more than twice as likely as other racial groups to have surgery and tend to have better outcomes when they do.
Many of us are interested in sorting out why these disparities exist. For example, Latinas present with more advanced prolapse. We are looking at the role of social stressors on health, as we know that stress can exacerbate urinary tract symptoms, and why Latinas tend to seek care much later when they have more severe symptoms. As doctors, we should be looking at all of this and trying to make things better for patients.
Additional Resources
Learn more about the Center for Female Pelvic Health at NewYork-Presbyterian/Weill Cornell Medical Center.
Larissa V. Rodríguez, M.D. is urologist-in-chief at NewYork-Presbyterian/Weill Cornell Medical Center and chair of the Department of Urology at Weill Cornell Medicine. An internationally renowned urologic reconstructive surgeon, Dr. Rodríguez specializes in the treatment of women with urinary and pelvic floor conditions, such as pelvic organ prolapse, stress urinary incontinence, genitourinary tract reconstruction, and chronic pelvic pain. Her clinical research focuses on outcomes of vaginal and robotic surgery, health disparities related to pelvic floor disorders, and the development and treatment of chronic bladder pain.
