When Should I Get a Bone Density Test?
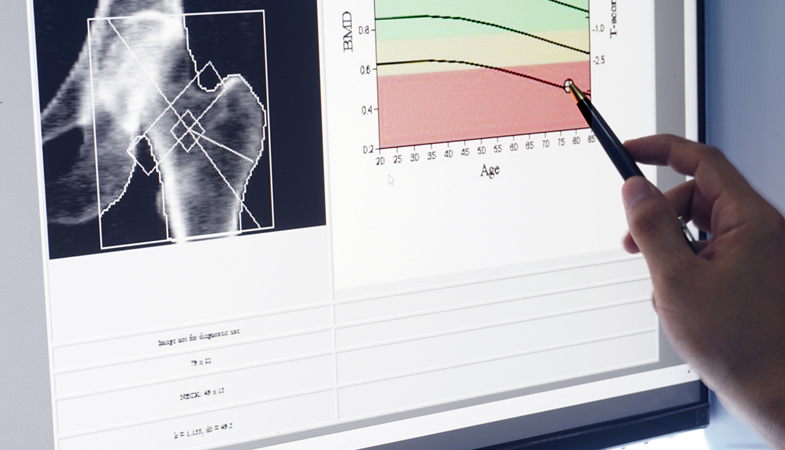
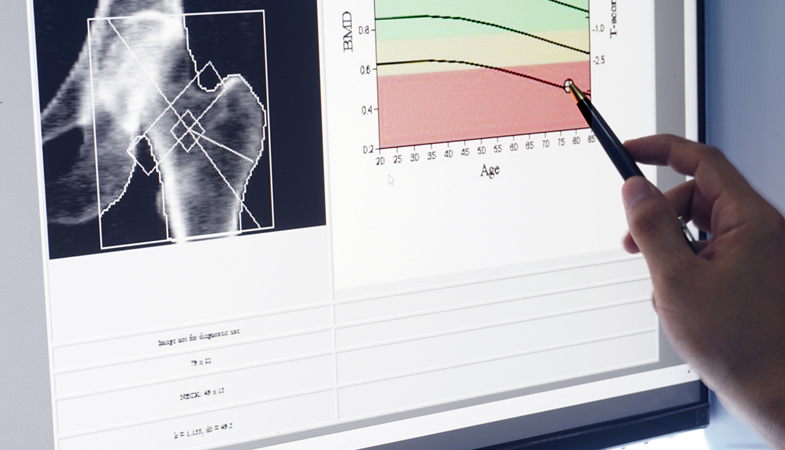
An expert explains how a DXA scan is a simple way to detect decreased bone mass and osteoporosis.
Bones, which are key to staying active and heathy, start to deteriorate in middle age. When the deterioration becomes severe, people can receive a diagnosis of osteoporosis, which translates to “porous bone.”
With osteoporosis, even a relatively benign activity — like wrestling a stubborn window open — can break a bone. The consequences of such fractures late in life can be profound, including pain, decreased mobility and function, and decreased quality of life.
“In older age, a very high percentage of people — more women than men — have osteoporosis or low bone mass,” says Dr. Marcella Donovan Walker, an endocrinologist at NewYork-Presbyterian/Columbia University Irving Medical Center. “One in three women over the age of 50 will experience a fracture related to osteoporosis in their lifetime.”
Changes from bone loss often go unnoticed. To detect decreased bone mass in the skeleton before the first fracture occurs, clinicians rely on the noninvasive scanning technology known as DXA (short for dual-energy X-ray absorptiometry and pronounced “dexa”). Dr. Walker shares what to know about bone density scans and who is most at risk for osteoporosis.

Dr. Marcella Donovan Walker
When to Get a DXA Scan
Guidelines for when to get a bone mineral density scan, and how often to repeat the scan, vary. The Bone Health & Osteoporosis Foundation recommends scans beginning at age 65 for women and 70 for men. Scans can begin even earlier, as early as age 50 for women and men who have risk factors for fractures. Dr. Walker assesses each patient’s risk to make personalized recommendations about when it’s time for a baseline DXA.
In women, bone mass drops most rapidly in the four to five years around menopause, when estrogen plummets, then slows and continues through the rest of life.
“Given that about 20% of women over age 50 have osteoporosis and 50% have low bone mass, getting a first scan around this age may be beneficial for people with risk factors,” says Dr. Walker, “because we have a chance to slow the loss before it gets worse.”
A wide variety of factors affect the rate of bone loss, says Dr. Walker, whose research investigates how certain medications speed or slow the process.
Osteoporosis risk is greater in people who take certain medications for cancer and epilepsy, certain blood thinners, or steroids. In all genders, a family history of osteoporosis, alcohol and tobacco use, or some medical conditions, including diabetes, increase one’s risk of fracture.
Based on your individual risk factors, your primary care provider can recommend when you should get your first bone density test.
DXA is Fast and Painless
Like a regular X-ray, a DXA scan uses low-dose radiation, is fast and painless, and doesn’t involve any injections. Plan on 15 to 20 minutes for the procedure.
DXA measures how much of the X-ray passes through the bone and converts this to a density measurement.
Results of the bone density test are sent to your healthcare provider, who will determine if treatment is needed.
What Happens If Your Bone Density Test Detects Bone Loss
Depending on the severity of bone loss, your healthcare provider may recommend watchful waiting or treatment.
The most widely prescribed treatments are a class of drugs known as bisphosphonates, which can be taken in pill form and slow bone loss. Another option — denosumab —requires an injection every six months. Some other injectable medications, such as teriparatide, stimulate bone formation. For younger people experiencing symptoms of menopause, hormone replacement therapy can slow the progression of bone loss.
“All drugs approved by the Food and Drug Administration for the treatment of osteoporosis reduce the risk of fracture. They are safe, and most people tolerate them without difficulty,” Dr. Walker says.
Ways to Help Prevent Osteoporosis and Slow Its Progression
Healthy eating: Your diet should be rich in calcium and vitamin D. Good foods include dairy, like milk and yogurt; certain green vegetables, like kale and broccoli; and fish, including sardines and salmon. Your doctor may test your blood and recommend calcium and vitamin D supplements.
Exercise regularly: Weight-bearing exercises — like brisk walking, low-impact aerobics, dancing, and climbing stairs — and resistance training such as using free weights, weight machines, and resistance bands are best for your bones.
Don’t smoke, and limit alcohol: Cigarette smoking and too much alcohol speed up bone loss and increase the risk of osteoporosis and fractures.
A version of this article originally appeared in the Columbia University Irving Medical Center newsroom.
Marcella Donovan Walker, M.D., is a professor of medicine in the Division of Endocrinology at Columbia University Vagelos College of Physicians and Surgeons and an endocrinologist at ColumbiaDoctors and NewYork-Presbyterian/Columbia University Irving Medical Center. She is board-certified in internal medicine and in endocrinology and sees patients in the Metabolic Bone Diseases Unit at Columbia University Irving Medical Center.

