Understanding the Risks of Stroke During Pregnancy
A neurologist explains why patients are at greater risk of stroke during and shortly after pregnancy, and how moms-to-be can recognize the signs and help reduce the risk of stroke.


With pregnancy being a time of so much change, health is often top of mind for moms-to-be. While many pregnant patients are aware of the risk of developing conditions such as gestational diabetes and high blood pressure, there’s one more health risk that should be on their radars: stroke during pregnancy, says Dr. Eliza Miller, a neurologist at NewYork-Presbyterian/Columbia University Irving Medical Center.
One in five strokes in women under age 35 are related to pregnancy, says Dr. Miller, who specializes in treating pregnancy-related stroke. “Stroke is something that can happen to a person at any age, and it tends to have different causes at different ages, but one of the major causes of stroke in young adults is pregnancy-related complications,” she says. “Thankfully, most of the underlying causes are treatable, and recognizing the warning signs early can greatly reduce the risk of stroke.”
Though these occurrences are rare, studies have shown the risk of stroke is nearly tripled in pregnancy, and that risk carries through in the weeks immediately following birth. Blood clotting, which can lead to stroke, occurs more frequently during pregnancy, and complications that lead to elevated blood pressure, such as preeclampsia and gestational hypertension, may raise the risk of bleeding in the brain.
For National Stroke Awareness Month, Dr. Miller, who is also an assistant professor of neurology in the Division of Stroke and Cerebrovascular Disease at Columbia University Vagelos College of Physicians and Surgeons, spoke to Health Matters about what pregnant patients should know about stroke.

Dr. Eliza Miller
Why does pregnancy increase the risk of stroke?
One cause is evolutionary. Historically, and still to this day, one of the biggest risks for maternal mortality is postpartum hemorrhage (bleeding) when you give birth, so our bodies have evolved to be very good at stopping bleeding. This can lead to an increased risk of developing blood clots. Rarely, this can lead to an ischemic stroke, where there is blockage of a blood vessel in the brain due to a blood clot.
The other major risk factor for maternal stroke is having hypertensive disorders of pregnancy, which are very, very common. Hypertensive disorders of pregnancy are when you develop elevated blood pressure in pregnancy or postpartum, so conditions like gestational hypertension, preeclampsia, or eclampsia. Even a healthy pregnancy puts a lot of strain on the heart and blood vessels, so having very high blood pressure adds to the strain on your arteries, and in extreme cases can cause them to burst. This is called a hemorrhagic stroke, and is a very dangerous form of stroke that is more likely to be fatal than an ischemic stroke.
What is the likelihood for stroke in pregnancy and postpartum?
Research has found that the risk of stroke is about 30 strokes per 100,000 deliveries, so it is overall a very low risk. In some groups — for instance, those with existing risk factors like chronic hypertension, heart conditions or genetic conditions that make them more likely to get blood clots — the risk might be higher during pregnancy, but generally it is not a common occurrence.
Pregnancy can be a time of high anxiety, so I don’t want to worry new mothers. However, being aware that stroke is a risk, being aware of the highest-risk time period, and being aware of the warning signs is important.
What are the stroke warning signs people should look out for during and after pregnancy?
I’m always concerned when people report they have a new or very severe headache, especially around that time of delivery or postpartum. Having migraines is actually a risk factor for developing preeclampsia, and it’s also a risk factor for stroke, so even if you have had headaches in the past, you should watch out for signs that this headache is different and might be more than just a migraine. If your headache is worse lying down than it is standing up, it’s a big red flag, because in general, a migraine usually gets better if you lie down in the dark in a quiet room. If you lie down flat and your headache becomes unbearable, that can be a sign of a blood clot. And if you have a headache coupled with high blood pressure, that’s a red flag.
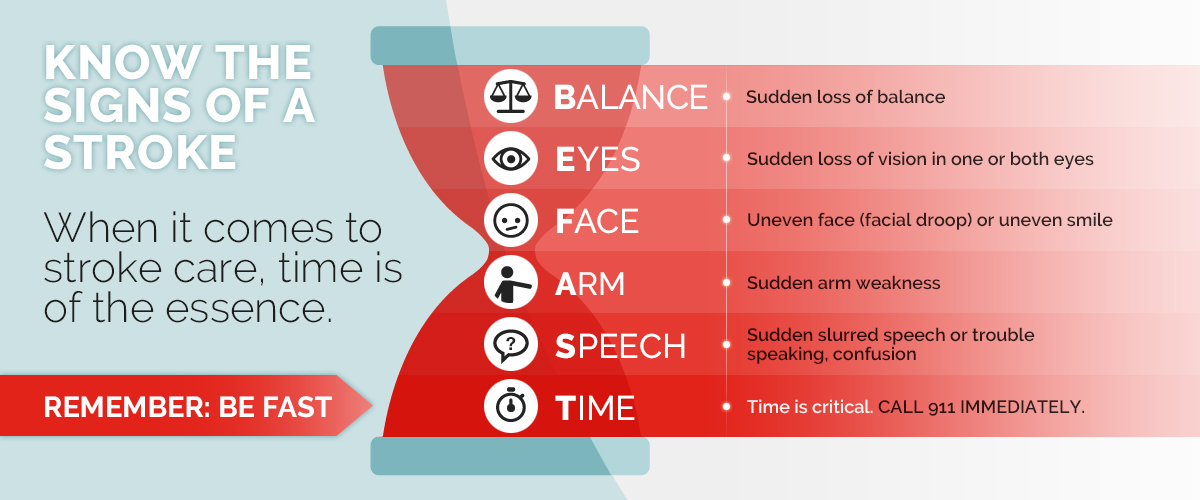
And of course, watch out for any of the typical signs of a stroke — numbness or tingling on one side, a droopy face, or slurred speech, or vision changes like loss of vision or double vision. We sometimes use the BE FAST mnemonic, which is Balance, Eyes, Face, Arm (weakness), Speech (difficulty or slurred), and then it’s “Time to call 911” because the quicker you get treated for stroke, the better the outcome. Time is brain!
Who is most at risk of stroke during pregnancy and after giving birth?
Anyone who has a hypertensive disorder during or after pregnancy is at risk, regardless of age or race. Between preeclampsia, which is a severe form of hypertensive disorder in pregnancy, gestational hypertension, which is like preeclampsia but less severe, and chronic hypertension (hypertension diagnosed before or early in pregnancy), almost one in 10 pregnancies is affected by some form of hypertensive disorder of pregnancy. Luckily, blood pressure is treatable, and it is one of the most modifiable risk factors for stroke in general.
There are also certain communities who are at higher risk. The risk of maternal stroke is up to two to three times higher if you are Black, Asian and Pacific Islander, or Latinx. I don’t believe this has anything to do with genetics. This is, unfortunately, most likely a product of systemic racism — a history of patients not having access to care, maybe not feeling safe in care, maybe not wanting to go seek care because they’ve had traumatic experiences with the healthcare system. I’ve had patients who don’t trust doctors because of previous experiences, but physicians talking with their patients about their experiences and listening to their concerns helps to keep communication lines open and build that trust so we can mitigate the risk of stroke.
When are you at greatest risk during your pregnancy?
The risk is highest in the immediate peripartum period, meaning the few days around delivery and the first couple weeks after. It gets lower and lower the further out you get. Some studies have shown that the risk remains elevated even up to a year after, but that depends on the individual patient, particularly those who have existing stroke risk factors.
“The risk of maternal stroke is up to two to three times higher if you are Black, Asian and Pacific Islander, or Latinx. ”— Dr. Eliza Miller
What can you do to reduce the risk of stroke during or after pregnancy?
Most importantly, check your blood pressure. If it’s high, we have safe medications that can lower your blood pressure. If we can prevent preeclampsia and treat gestational hypertension when it occurs, then we can lower the risk of stroke. In addition, in general you can lower your risk of stroke throughout your life by staying active, exercising, stopping smoking, and eating a healthy diet such as the Mediterranean-type diet. I tell my patients, if you cook it yourself, it’s generally going to be better for you than if it comes in a package or you get it from a restaurant or fast-food place.
It’s also important to recognize certain warning signs in case they may be more than just being tired or having a headache from lack of sleep due to having a newborn baby in the home. Blood pressure is sometimes called the “silent killer.” It’s one of those things that I really wish that it hurt, because if it hurt, people would be much more aware of it.
What are the signs that your blood pressure might be too high?
If you’re not feeling well in the period right around the time of delivery or afterward, especially if you have a headache, then check your blood pressure. In many young women, their normal blood pressure is pretty low, like 90 over 60, so if your blood pressure is usually low and now it’s 140 over 85, that’s really high for you, and you should call your doctor.
It’s important to note that rising blood pressure doesn’t happen out of nowhere. It happens over a period of time, usually a few days. If you notice some days the top number is 120 and some days it’s 110, that’s fine. If it’s persistently a little bit higher, like creeping up toward 130, then that’s something you need to talk to your doctor about even if you’re young. Anything over 120 over 80 is actually considered elevated.
Can you check your blood pressure at home?
Yes. You need a blood pressure cuff, and if you’re pregnant, you need a particular cuff that has been validated for pregnancy, so you should talk to your obstetrician about that.
What else can the healthcare community do to address the risk of stroke caused by pregnancy?
One thing that I’ve tried to do in addition to educating the public and patients about risk factors and warning signs is to get more of a conversation started between the world of obstetrics and the world of neurology and build a better understanding of pregnancy and stroke. Collaboration between these specialties is key. I see patients in a special neuro-obstetrics clinic at The Mothers Center at NewYork-Presbyterian/Columbia University Irving Medical Center, which is a space dedicated to providing coordinated care to pregnant patients with complications requiring specialized care. The Mothers Center is a good model for addressing stroke in pregnancy because it makes it so much easier to collaborate with my colleagues in obstetrics. I see a lot of the high-risk patients, and do patient education about the risk of stroke during and after pregnancy, and manage any neurological complications that might come up for our patients. I also see patients there who might have had a stroke in the past and now are pregnant or planning a pregnancy, and we talk about how we will work together to prevent complications. Working with the Mothers Center has been one of the most rewarding parts of my practice, and we are continuing to expand our pregnancy-related stroke work together, both clinically and on the research side.
Additional Resources
For more on pregnancy-related stroke and other stroke services at NewYork-Presbyterian, visit nyp.org/neuro/stroke/pregnancy-related-stroke
If you’d like to learn more about NewYork-Presbyterian’s services for pregnant individuals needing specialized care, visit The Mothers Center.

