Understanding Multiple Sclerosis: What to Know about MS Symptoms and Treatments
A neurologist explains who is most at risk for this condition and ways to manage the symptoms.

Multiple sclerosis, commonly referred to as MS, is an autoimmune disease that attacks a person’s central nervous system. It can lead to a wide variety of symptoms, such as tingling, numbness, weakness, visual disturbance, and balance changes. Depending on the severity of the damage to the central nervous system, a small percentage of people may lose the ability to walk independently. Approximately 1 million people in the United States live with MS, according to a 2019 study from National Multiple Sclerosis Society, which was nearly double the previous estimates.
This chronic condition has no cure, but there have been large advancements in treatments to change the course of the disease and help people maintain their quality of life, says Dr. Karen Blitz, a neurologist and director of the Multiple Sclerosis Center at NewYork-Presbyterian Brooklyn Methodist Hospital.
“We are so much better at treating this disease than we were 30 years ago,” says Dr. Blitz. “We have so many treatment options.”
For MS Awareness Month in March, Health Matters spoke with Dr. Blitz, who is also an assistant professor of clinical neurology at Weill Cornell Medicine, to learn what patients, families, and caregivers should know about living with this disease.
Dr. Karen Blitz
What is multiple sclerosis?
Dr. Blitz: Multiple sclerosis occurs when the immune system becomes misguided and attacks the central nervous system, which includes the brain and spinal cord. This can inflame and scar the central nervous system and damage the protective insulation — called the myelin — that surrounds nerve fibers. Inflammation and damage to the nervous system can impact communication between the body and brain and causes MS symptoms.
What are the symptoms?
The most common symptoms include loss of vision in one eye, double vision, difficulty walking, fatigue, numbness in the face or extremities, dizziness, bladder or bowel problems, or even cognitive issues. The symptoms can mimic other neurological diseases and are so varied depending on the location of the inflammation or nerve fiber damage and level of deterioration that it can be difficult to identify MS right away.
Does this mean it’s easy to overlook symptoms of MS?
Yes. Someone could experience vision loss in one eye and before they have a chance to see an ophthalmologist, the symptom is gone. Or a parent might notice their kid had trouble walking at the age of 10 for a day or two, but then it went away until something triggered it again 10 years later. What’s important is noticing if any unusual symptoms last more than 24 hours. If someone wakes up and their hand is numb and it goes away after a few minutes, that’s probably not MS. But if numbness, balance, vision issues, or any other symptoms associated with MS last for 24 hours or more, that person should see a neurologist.
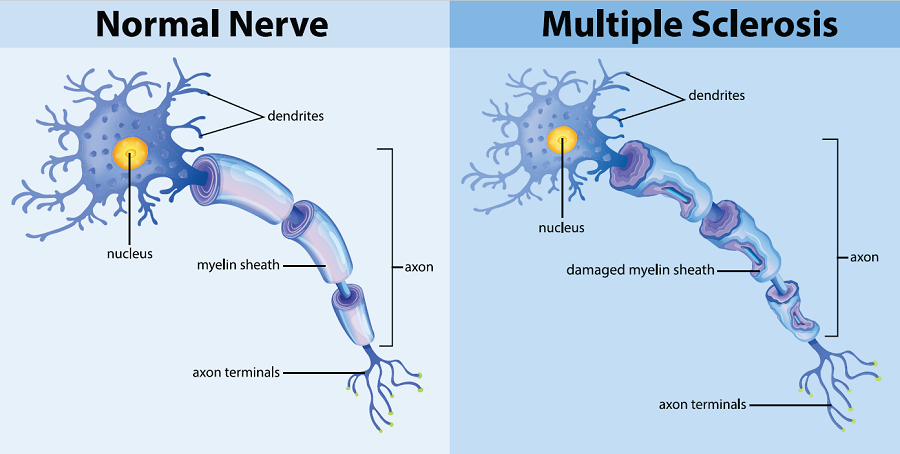
A normal nerve compared to a nerve with damage to the insulation that protects the nerve. This damage can impact communication between the body and brain and causes MS symptoms.
How is MS diagnosed?
There’s no test to definitively diagnose MS. But your doctor will take a full history, including asking about previous symptoms, and perform a neurologic exam. They would likely order an MRI to look for damage to the central nervous system, or do a spinal tap to look for evidence in a person’s cerebrospinal fluid.
Who is most at-risk for MS?
People with certain genetic makeups are more predisposed to MS, and infections can trigger the change in the immune system that causes MS. Environmental factors can also play a role. Low vitamin D may increase the risk of MS, and smoking may worsen the disease progression. But we don’t know why it’s triggered in some people and not others. It’s most commonly diagnosed between the ages of 20 and 40, but can be diagnosed anywhere between the ages of 10 and 70. It is three times more common in women than in men.
Can MS be cured?
Unfortunately there is no cure for MS. But there are numerous medications and rehabilitation options to help manage the disease. And patients can maintain their own wellness through exercise, avoiding smoking, and maintaining a healthy diet. Our job as health care practitioners is to calm down the immune system so patients don’t have a relapse, and the patient’s job is to stay actively involved in their treatment by taking their medications and making the necessary lifestyle changes. This is a lifelong disease that will require lifelong treatment.
What are the treatment options?
Treatment plans are often a combination of medications tailored to the individual patient. More than 20 medications exist to treat this disease. Steroids are often used to reduce inflammation after an attack, while other medications, known as disease modifying therapies, are used to reduce the number of attacks and slow the disease progression. Balance or speech problems, for example, can be managed through physical therapy, speech therapy, and exercise. Occupational therapy can assist with cognitive issues and with activities of daily living, such as walking, dressing, and bathing. Everyone with MS should be treated early and they should stick to their treatment plan because there is good data to show people who adhere to their treatments have a lower likelihood of experiencing a relapse.
Types of MS
MS affects people differently. Doctors classify the disease into 4 categories. A small number of patients will have a completely benign form of MS, but many will experience a variety of symptoms and relapses over time and may experience worsening problems, potentially losing their ability to walk without the assistance of a cane or wheelchair. Patients should be armed with the basic information about MS by their practitioner because this knowledge can help patients know what to expect as they, their doctor, and their family work together to find the best treatment.
Clinically isolated syndrome refers to a single episode of MS symptoms that lasts at least 24 hours, followed by a complete or partial recovery. People with CIS may or may not go on to develop MS.
Relapsing-remitting is the most common type of MS, which is diagnosed in about 85% of people with MS. In this type, a person will suffer an attack (relapsing), followed by a period of recovery (remitting). A relapse can last for days or weeks, and periods of remission can last for weeks, months, or years.
Secondary progressive can occur in some people who have had relapsing-remitting MS for years. This happens when their symptoms begin to get steadily worse over time.
Primary progressive, the least common, is progressive from the start. The symptoms, which are usually characterized by walking problems and fatigue, become steadily worse with no periods of remission.
For people with relapsing-remitting MS, what causes a relapse?
We don’t know why the disease will go quiet, but we do know that the immune system can be activated and cause patients to have new symptoms. Many MS patients are heat-intolerant so if they spend time in a hot room, that can exacerbate the symptoms. Similarly, fever from an infection, like the flu or COVID, increases the body temperature and can cause symptoms to recur. Smoking has been shown to increase the risk of disability , while lifestyle changes like adhering to a low salt diet, limiting stress, and getting exercise can help prevent a relapse. But it’s going to be different from person to person.
What should families and caregivers know about caring for someone with MS?
MS is rarely fatal, but as a chronic, lifelong disease, patients need a good support system to work with them through the ups and downs of this illness. Emotionally this can be harder if the person is diagnosed as a child or teenager.
Family and friends can play an important part in keeping patients on the right track. They can make sure their loved one has exercised that day, taken their medication, stayed well-hydrated. Family members or caregivers are often very astute in noticing if a patient is limping or is having cognitive issues that would indicate an exacerbation of the disease. Any kind of support so the patient knows they are not in this alone is helpful.
Karen Blitz, DO, is a neurologist at NewYork-Presbyterian Medical Group Brooklyn, assistant professor of clinical neurology at Weill Cornell Medicine, and the director of the Multiple Sclerosis Center at NewYork-Presbyterian Brooklyn Methodist Hospital. She specializes in the treatment and management of patients with multiple sclerosis and has a special interest in neurorehabilitation. Dr. Blitz evaluates patients with neurological disorders to develop treatment plans to optimize function and mobility.
Additional Resources
Learn more about the services available at the Multiple Sclerosis Center at NewYork-Presbyterian Brooklyn Methodist Hospital.
For more on neuroscience services at NewYork-Presbyterian, visit www.nyp.org/neuro.
