Helping the Voiceless Express Themselves
NewYork-Presbyterian Chaplain Joel Berning’s communication board gives ICU patients the chance to convey their spiritual needs.
To understand how Joel Berning’s spiritual care communication board came to be is to follow the advancements of modern medicine.
Ten to 20 years ago, patients who were critically ill, on mechanical ventilation, and unable to speak, would have been sedated.
“But in the last decade, the best practices in the ICU, in critical care, have moved to sedating people less because, if you keep them awake, they can participate in their care and have better outcomes,” says Berning, a chaplain at NewYork-Presbyterian.
It was while tending to these patients, who are awake but breathing through a tube, that Berning realized they needed a way to communicate their spiritual needs. In 2013, he began working on creating the board, which is modeled on nursing communication boards.
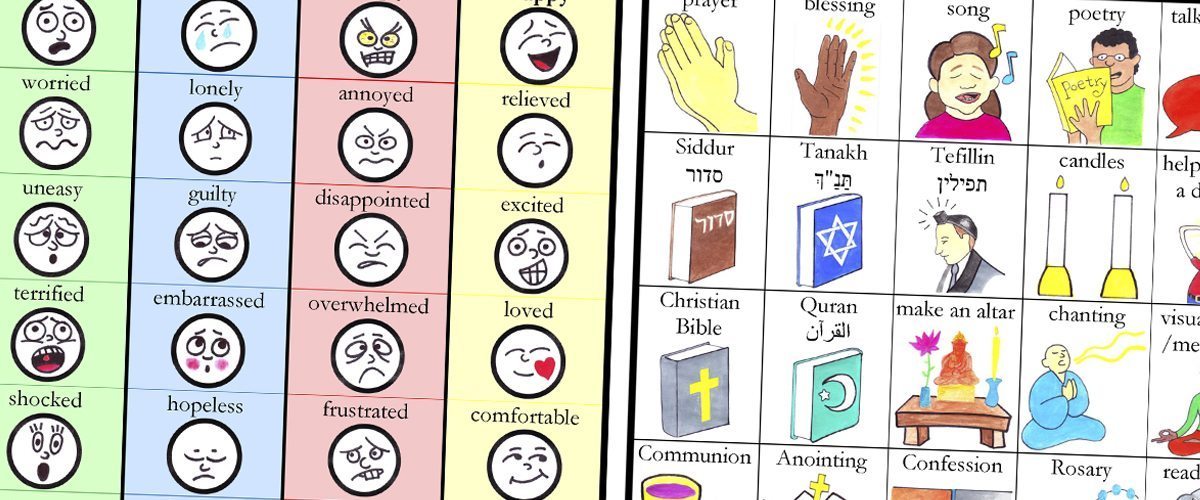
By March 2014, Berning had a working prototype and began to test it among 50 mechanically ventilated adults in medical or surgical ICUs to determine if receiving this spiritual care works. The board reflects the four areas of spirituality that would be assessed by a chaplain: religious affiliations, feelings, spiritual pain, and a desired religious or nonreligious intervention a chaplain can provide, like needing prayer or a hand held. Berning then collaborated with his colleague Seigan Ed Glassing, a Buddhist chaplain and former graphic designer, who developed illustrations of the interventions and cartoon faces for the emotions, so patients could more easily identify their feelings and needs by pointing to them.

Joel Berning
In conjunction with other NewYork-Presbyterian doctors and clinicians at Columbia University Medical Center, Berning’s research partners — including Dr. Matthew R. Baldwin, attending physician in Critical Care Services at NewYork-Presbyterian/Columbia University Medical Center and assistant professor of medicine at Columbia University Medical Center — measured how much anxiety someone was experiencing before and after using the spiritual care communication board. They did this by having patients use a visual analogue scale, a tool that measures subjective feelings like pain.
“On average, patients’ feelings of stress and anxiety went down 31 percent,” says Berning. “Then we did follow-up interviews, and 80 percent of the patients that we interviewed said it helped them feel more capable of dealing with their hospitalization.”
At the end of 2016, Berning finalized the spiritual care communication board and, with the help of NewYork-Presbyterian’s NYP Ventures, a strategic investment fund that supports advancements in digital services and innovations in health care, has licensed it to be produced in English and Spanish for distribution at hospitals throughout the country.
“People in the ICU have a variety of different experiences in the hospital just like any other group of patients,” says Berning. “With this tool, we are able to actually see — and get at — what is happening for them.”
