Rachel’s Journey to a New Heart
For years, Rachel Harper lived with heart failure that grew increasingly worse. Then, the cardiovascular care team at NewYork-Presbyterian/Columbia University Irving Medical Center earned her trust and helped turn her health around.
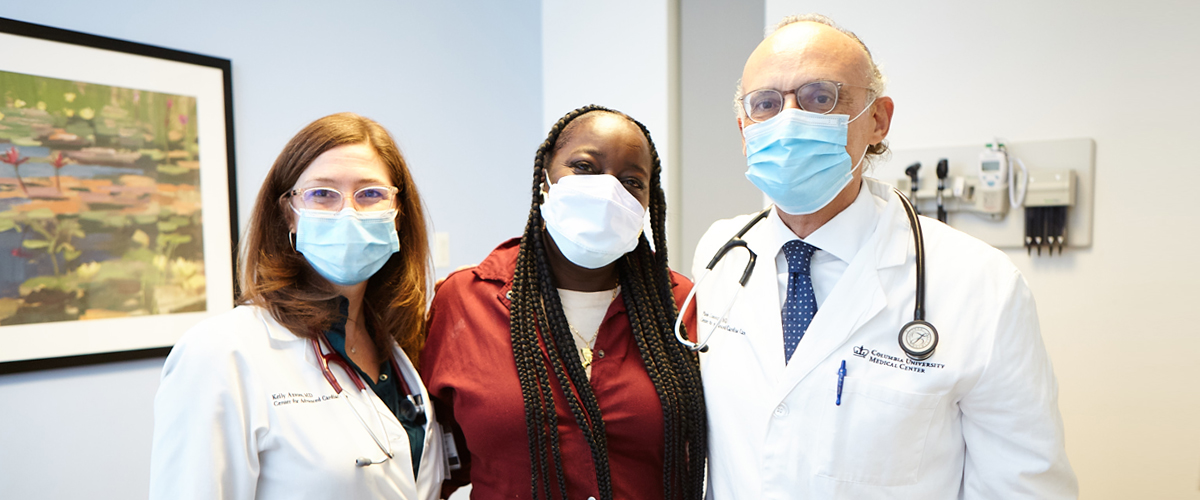
Patient Rachel Harper (center) with cardiologists from her NewYork-Presbyterian/Columbia care team, Dr. Kelly Axsom (left) and Dr. Paolo Colombo.
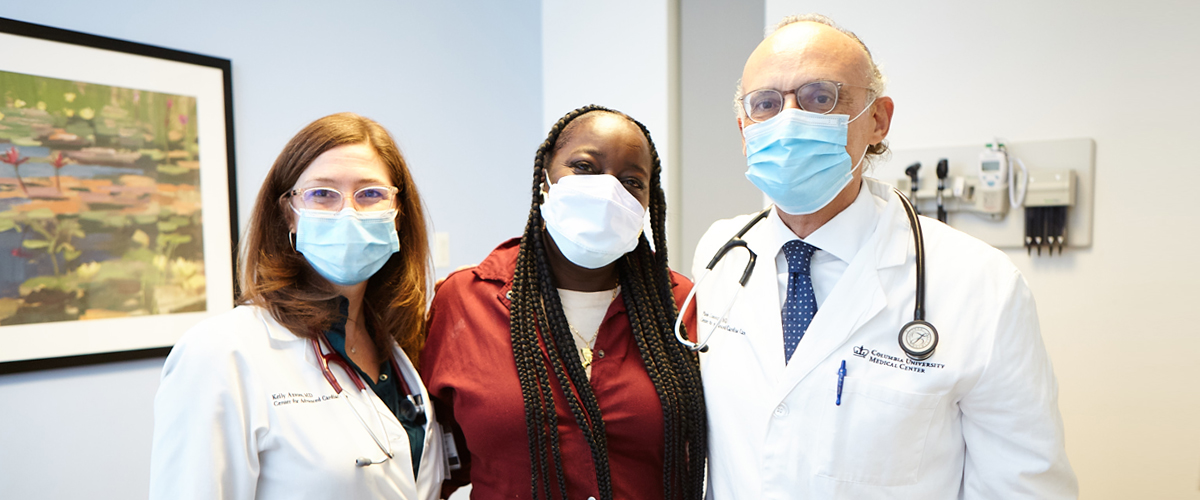
Patient Rachel Harper (center) with cardiologists from her NewYork-Presbyterian/Columbia care team, Dr. Kelly Axsom (left) and Dr. Paolo Colombo.
Rachel Harper was no stranger to having tough conversations in doctor’s offices, being a cancer survivor and having lived with familial cardiomyopathy, a genetic disease of the heart muscle that often left her feeling weak and out of breath. Still, the 51-year-old mother of four struggled to process what her cardiologist told her at an appointment in 2019. After running some tests, her care team had discovered that Rachel’s heart failure was rapidly progressing, and she was in need of more serious intervention.
“Rachel, you are dying,” Dr. Kelly Axsom, medical director at NewYork-Presbyterian’s Centralized Heart Failure Management Program, remembers telling her. “But I’ll be damned if I let you die in front of me. You are a strong woman. You have so much to live for.”
Dr. Axsom presented her with two options: get a left ventricular assist device (LVAD), a surgically implanted heart pump that would help her weakened heart until she was able to get a transplant, or begin hospice care.
“I didn’t want to hear it,” Rachel admits, recalling how she stormed out of the appointment. “I didn’t want to make a choice.”
When she got home that day, Rachel cooled down and thought about how far she had come. In and out of local hospitals for years, she had been so sick that she could barely eat or stand up straight. Her family encouraged Rachel to seek care at NewYork-Presbyterian/Columbia University Irving Medical Center, and it was only then that she began to see improvement in her heart failure symptoms.
“My progress started at NewYork-Presbyterian,” Rachel says. “They took a chance on me, and I decided to come back and take that same chance.”
Rachel went back to the hospital and decided to undergo the LVAD implantation in August 2019, beginning her journey to a healthier life and a new heart.
Fighting to Get Healthy
From the age of 35, Rachel had been living with health challenges. She had a defibrillator implant to detect and stop irregular rhythms for her weakening heart. Her heart condition had also led to a clot in her heart, which caused a stroke. Apart from her cardiac issues, she was diagnosed with lymphoma in 2016 and underwent cancer treatment.
With her health failing — she had been hospitalized more than 20 times — she went to NewYork-Presbyterian/Columbia University Irving Medical Center in 2017, hoping doctors could finally get her on the right path.
“I had been to other [hospitals] where they called me a hypochondriac,” Rachel recalls. “For years, other places couldn’t treat what was wrong with me.”

Dr. Kelly Axsom
“She had very low heart function and was in dire straits,” says Dr. Axsom, who is also an assistant professor of medicine at Columbia University Vagelos College of Physicians and Surgeons. “But she was tough, and we wanted to fight for her.”
The NewYork-Presbyterian team helped stabilize Rachel’s heart function with medication and implanted a small sensor device to remotely monitor any changes. She received additional care for recurrent bouts of pneumonia, along with follow-up from oncologists, Dr. Axsom explains.
“When I started seeing Dr. Axsom and her team, it was a thousand percent turnaround.” Rachel says. “As time went on, I started sitting up straight, I was able to stand up, I was able to eat. We had different new treatments and they tried everything.”
But in 2019, her health took a turn for the worse again.
Due to her history with cancer, Rachel was a high-risk candidate for transplant. Doctors wanted her to be disease-free and give her body an opportunity to heal. An LVAD, a mechanical pump that helps the heart’s bottom left chamber pump blood through the body, was her best chance to reduce heart failure symptoms and offer lifesaving support.
“At first, I didn’t want it, but my family and my doctors helped me through. They were so good to me,” she says. “I thank God for them.”

Rachel customized fanny packs for her LVAD battery, embracing the device as part of her life.
From Apprehension to Advocacy
Following her procedure with cardiac surgeon Dr. Yoshifumi Naka, surgical director of heart failure, heart transplantation, and mechanical circulatory support programs at NewYork-Presbyterian, Rachel’s world opened up: Bike rides through Central Park, roller-skating, cheering on her son at basketball games, having dinner with family — she enjoyed all the simple pleasures she had missed for years.
She quickly embraced the LVAD as a part of who she was, customizing and bedazzling fanny packs to carry the external battery for everyday use and special events like her daughter’s wedding.
Rachel was eager to pay it forward. After getting her LVAD, she became an advocate for patients considering the treatment, sharing her experience with others.
“She talks about the fear, her difficulty accepting what she needed,” Dr. Axsom says. “The patients find such community in it.”
“I want people to understand that it’s not a death sentence,” Rachel says. “That LVAD made me feel like I had a whole new heart.”
Rachel lived with the LVAD for three years.

Rachel received a new heart on January 5, 2022.
A New Heart
Then, in 2021, Rachel experienced an infection in her driveline, a connector that extends from the internal device to the controller outside of the body. This posed a risk of greater illness, and was coupled with a complication in the LVAD that was preventing the flow of blood.
Fortunately, Rachel had reached a point in her post-cancer recovery where her care team felt confident that she was ready for the next chapter in her journey: At the end of December, she was placed on the national waiting list for a heart transplant. After a five-day wait at the hospital, Rachel received news of a donor heart, and on January 5, 2022 she underwent a successful four-hour surgery led by Dr. Yuji Kaku, surgical director of the Cardiogenic Shock Program at NewYork-Presbyterian/Columbia University Irving Medical Center.
When she woke up, the first thing she looked for was her LVAD.
“I cried like a baby,” Rachel says. “It became part of my life, it was there with me all the time.”
The initial weeks of post-transplant recovery were difficult and taxing on her body, she recalls, but within months, she was feeling stronger and looked forward to making plans with her family and friends.
Throughout her health challenges, Rachel continued to make the best of every situation, bonding with her care team during her hospitalization.

Dr. Paolo Colombo
“Rachel is one of those people that looks at things from the positive side, and understands that without this evolution in medicine — the LVAD and transplant — she would not be alive,” says Dr. Paolo Colombo, medical director of the Mechanical Circulatory Support Program at NewYork-Presbyterian/Columbia University Irving Medical Center and professor of cardiology at Columbia University Vagelos College of Physicians and Surgeons. “She is an exceptional person. Her energy and attitude are really unique and helped her recover not only physically, but mentally.”
The collaboration and compassion between a patient and their care team is key, Dr. Axsom adds.
“Our team recognizes that patients need time to make really big life decisions, and we need to be there to support them not just in the big, crash moments, but through thick and thin,” she says.
Moving Forward
In the year after her transplant, Rachel has gone dancing and bowling with her four children, and traveled to Jamaica and Florida to spend time with family. The 2022 holiday season at the Harper household was one to remember, as Rachel cooked up a feast for her family for the first time in seven years.
While she marked her first post-transplant birthday on August 23, she had no big plans. Instead, she waited until the new year, which she rang in with a cake and a small party with her close family.
“My new birthday is January 5. That’s what I’m celebrating from now on,” Rachel says of her heart transplant date.
Amid it all, she still finds time to lend a helping hand to her neighbors, opening a new food pantry in the Bronx after helping run a separate location in the borough for 19 years.
“I’m so appreciative of what NewYork-Presbyterian has given me, so I have a lot of love to share with everybody else,” she says.
“I’m blessed. From having a stroke, my heart, pneumonia, the chemo, the LVAD, my chest opened twice — to still be standing? I’m grateful for everything, to have just one more day.”
Additional Resources
Learn about our comprehensive cardiovascular services.
See more about NewYork-Presbyterian’s expanded heart transplant and heart failure services.

