Long COVID: What We Know Now
Two experts share what we’ve learned about long COVID, including common symptoms, who is most at risk, and ways to treat the condition.

Hundreds of millions of people have had a COVID-19 infection, and many continue to face lingering symptoms, known as long COVID. A recent long COVID report that studied nearly 100,000 people in Scotland found that 6% had not recovered from COVID-19 up to 18 months after infection. About 42% reported partial recovery in that time span.
“This report reiterates that post-COVID complications are common, especially neurologic and cardiopulmonary symptoms,” says Dr. Lawrence Purpura, an infectious diseases specialist at NewYork-Presbyterian/Columbia University Irving Medical Center. Purpura, who treats patients with severe long COVID symptoms in his clinic, has established a study that looks for risk factors for developing long COVID, as well as reasons for why long COVID happens in the body and potential future diagnostic tools.

Dr. Lawrence Purpura
While awareness of long COVID has increased, allowing clinicians to refine their approach to diagnosing and treating patients, researchers are still looking for a more standardized definition of long COVID — and for clues to help predict who will develop it and how long they may take to recover.
We spoke with Dr. Purpura and Dr. Sarah Ryan, a primary care physician at NewYork-Presbyterian/Columbia University Irving Medical Center who also treats long COVID patients, about what they’ve learned about the condition.
Dr. Sarah Ryan
The Scotland study closely examined long COVID symptoms. Are you seeing similar symptoms in your long COVID patients?
Dr. Purpura: Yes, the findings from the study are similar to what I am seeing in my clinic. Many patients are presenting with brain fog, palpitations, fatigue, sleep disturbance, shortness of breath, and mental health problems, all of which are reported in the long COVID study from Scotland. In general, patients who are fully vaccinated or who had a very mild acute infection are less likely to present with severe long COVID symptoms, but I still encounter a few of those new patients a month.
Dr. Ryan: In my primary care practice, I do see people who had mild or asymptomatic COVID that then developed vague symptoms a few months later. The most common symptoms are decreased exercise tolerance, fatigue, and brain fog. I think many of my patients are not necessarily making the connection that their symptoms are a result of COVID. They come in for specific concerns, and, after a thorough assessment, we come to the conclusion that it might be due to the COVID infection. In most of these patients at my clinic, I see near full recovery after 6 to 12 months.
How has long COVID changed over the past two years?
Dr. Ryan: When COVID first started, a lot of people were hospitalized for COVID pneumonia. Many were on a ventilator for a long time. So perhaps the severity of the illness and duration of the hospital stay contributed to their long COVID. It’s hard to know whether symptoms like muscle and respiratory deconditioning were due to hospitalization or COVID.
Dr. Purpura: Fortunately, we’re seeing less severe long COVID in the past several months. There are a few reasons contributing to this. First, it’s been shown that vaccination can help prevent long COVID. I also suspect that the new Omicron variants have mutated to the point where they’re acting very differently than the original virus and the Delta variant. The Omicron variants are mostly causing mild upper respiratory infections, especially in those who are fully vaccinated, so in patients who were infected with Omicron, we’re seeing fewer long-term pulmonary complications, fewer neurocognitive issues, and fewer symptoms such as increased heart rate, lightheadedness, and chronic fatigue.
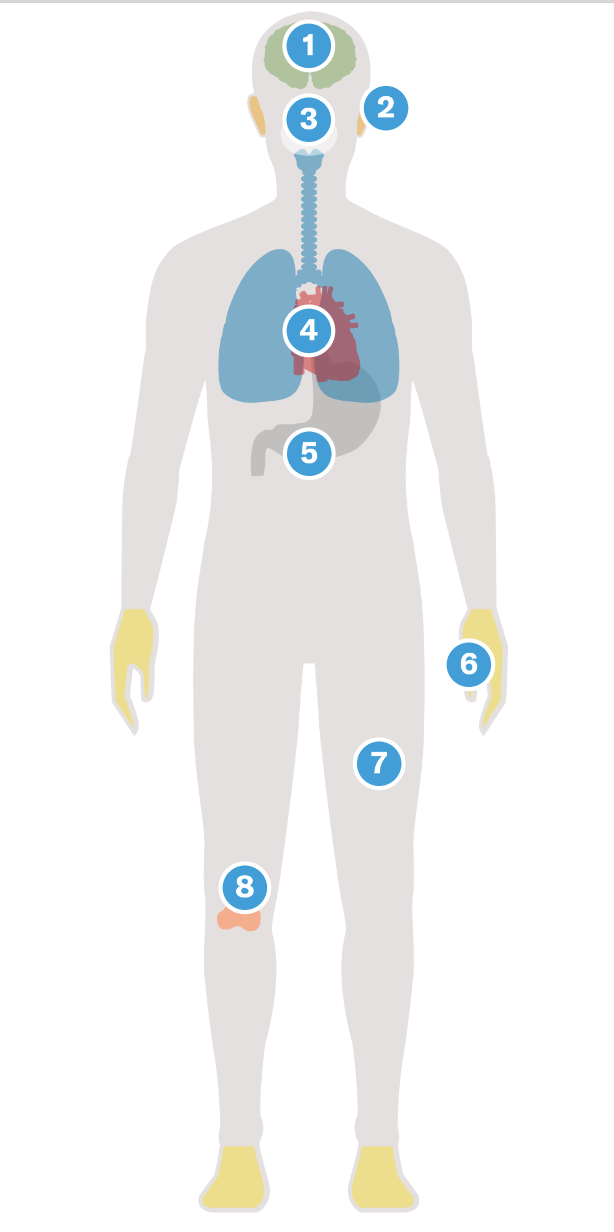
The condition can lead to a range of lingering symptoms.
-

Brain
Symptoms can include problems with concentration and memory, anxiety, depression, dizziness, fatigue, and insomnia. -

Ears
Some patients have reported ringing in their ears. -

Tongue & Nose
Symptoms can include a loss of taste and smell. -

Heart
Patients have reported feeling an increased heart rate. -

Digestive System
Symptoms can include nausea, diarrhea, and constipation. -

Hands & Feet
Patients have reported feeling tingling, discomfort, and a numbing sensation. -

Skin
Symptoms may include hives and a rash. -

Muscles & Joints
Some patients have reported muscle weakness and joint pain. "For the majority of long COVID patients, the good news is that many have profound recovery by three to six months after their symptoms," says Dr. Lawrence Purpura.
How many people develop long COVID after their initial infection?
Dr. Purpura: This is a tricky question to answer. It depends on how long COVID is defined. A lot of research studies use the criteria of having at least one symptom for more than 12 weeks after the acute infection. This definition is very broad and includes a lot of people who only report very mild symptoms such as mild fatigue or chronic nasal congestion. Studies that use a liberal definition report that between 20% and 80% of COVID patients develop long COVID, but those studies probably overestimate how many people have moderate to severe long COVID. Furthermore, many long COVID symptoms are commonly caused by other chronic conditions, so it is important to confirm that they are actually due to COVID infection.
In reality, I think the burden of moderate to severe long COVID is much lower, along the lines of 1% to 5%, across all variants. In our study with Columbia colleagues Michael Yin, Anne-Catrin Uhlemann, and David Ho, we find that at 12 weeks around 25% of COVID patients with lingering symptoms reported fatigue, 25% reported insomnia, and around 20% reported increased heart rate or dizziness, but only 15% reported neurocognitive deficits like difficulty with short-term memory. It is also important to note that the severity of these symptoms ranges from very mild to severely disabling.
Do we know what causes long COVID?
Dr. Purpura: There are several hypotheses about what causes long COVID. It’s thought that the initial COVID infection triggers an inflammatory cascade that produces lingering symptoms. We are looking for biological indicators, like autoantibodies, immune markers, or specific proteins in the blood that could be used to screen for long COVID. We are hoping these biomarkers can potentially help us track the disease course over time and evaluate efficacy of treatment.
We are also investigating the possibility of viral persistence. Most people clear the virus from their respiratory tract quite quickly, and the virus is usually undetectable by PCR testing after a few weeks. However, it is theoretically possible that the virus becomes dormant in different areas of the body and reactivates to cause long COVID symptoms, although we have not seen evidence to support this theory. Another hypothesis is that COVID infection may reactivate other viruses, specifically Epstein-Barr virus, and that reactivation leads to long COVID symptoms.
"Studies show that even one dose of a COVID vaccine reduces the odds of developing long COVID by seven to 10 times."— Dr. Sarah Ryan
Who is at risk of developing long COVID?
Dr. Ryan: We have come a long way since March 2020, but there’s a lot we have to learn about COVID itself and long COVID. One article I refer patients to, published in Cell, identified four factors that correlate with greater risk of long COVID — type 2 diabetes, prior infection with Epstein-Barr virus, level of SARS-CoV-2 RNA detected in the blood, and the presence of autoantibodies.
Many of the people I see are young, with no prior health conditions. These are folks who are at the peak or beginning of their career, and when you think about [the impact of long COVID on] quality of life and productivity, we are talking about a very costly condition in the long run.
Studies show that even one dose of a COVID vaccine reduces the odds of developing long COVID by seven to 10 times. I highly recommend that my patients get vaccinated and boosted.
Do people with long COVID get better? Are there any treatments?
Dr. Purpura: The first approach to treatment is lifestyle modification. We start by making recommendations that people can implement immediately. Monitoring diet or making changes based on which foods might cause flare-ups is something we include in our initial counseling. For example, many people report acute worsening of their symptoms with specific foods, such as meat, processed carbohydrates, and alcohol, so we recommend smaller meals throughout the day, and plant-based and low-inflammatory diets.
We have found a few other non-pharmacologic interventions that can often help. For people with dizziness, staying hydrated and supplementing with electrolytes has really helped. We can also recommend compression stockings to make sure they are keeping adequate blood flow to the brain.
For the majority of long COVID patients, the good news is that many have profound recovery by three to six months after their symptoms. Probably less than 10% have symptoms for longer than a year, and an even smaller percentage are still having symptoms that are considered moderate or severe for more than a year and half.
Dr. Ryan: I do think that many people with long COVID get better over time, and most data point to gradual improvement for many. However, the recovery can be slow, with bouts of setback.
The lesson learned is that despite the milder Omicron variant, COVID is still a public health threat, and long COVID poses a great challenge not just at the level of personal health, but our economic recovery from the pandemic, with many Americans unable to return to work due to long COVID. The best solution is continuing to encourage vaccination and boosting, which will reduce the chances of people developing long COVID symptoms.
A version of this article originally appeared in the Columbia University Irving Medical Center newsroom.

