Kim’s Gift: How a Sister, Adopted From Vietnam, Gave Her Brother a Chance for a Better Life by Donating a Kidney
Duncan Chinnock never imagined that his adopted sister, Kim, could be his organ donor. But organ donors don’t have to be a perfect match as Duncan discovered.

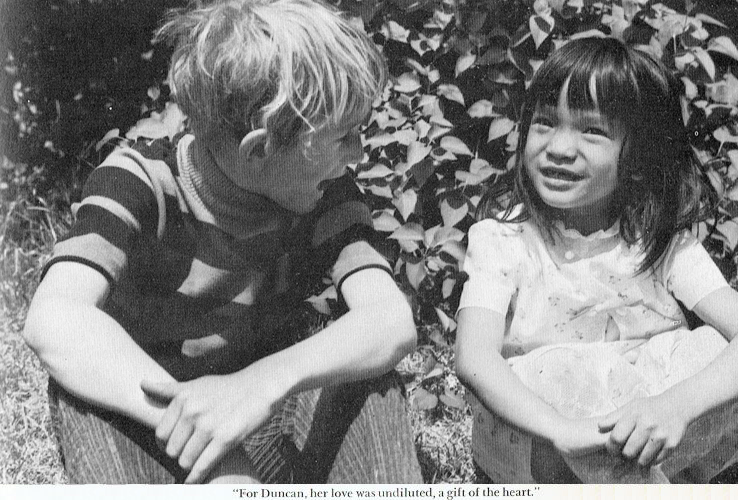
When Duncan Chinnock was 6 years old, he learned that his parents, Frank and Jan, were hoping to adopt a little girl from Vietnam. One of his first questions, to his journalist father, was, “Can I be her favorite?”
“Her favorite will have to earn it,” Frank gently told his son. Ultimately, the adoption took 19 months from the day Frank spotted Kim in an orphanage in Saigon, where a police officer had brought her after finding her wailing and severely malnourished amid the rubble of a bombed-out building.
Kim wasn’t in much better shape when she arrived at the Chinnocks’ rambling colonial in Katonah, New York, on November 11, 1967. As Duncan, now 59, remembers it, “She had health issues from the beginning,” including dormant tuberculosis, a perforated eardrum, and lice. “Two or so years in an orphanage took a toll,” he says. Still, Duncan took Kim’s hand and led his silent, unsmiling sister to her new room. They couldn’t talk since Kim didn’t speak English. Instead, he began to entertain her with a wind-up train, making Kim laugh for the first time that afternoon with a series of pratfalls. “We were close in age and I was very excited to have a younger sibling,” says Duncan, who has two older brothers, Chris and Randal. “We would pal around together, and in the beginning, when she had terrible nightmares, I would go to her room and try to comfort her.”
Kim, now 55, recalls the two of them playing with G.I. Joes and building forts with blankets in Duncan’s bedroom, and lying with him in the back of the family station wagon, looking out at the stars. But mostly, she remembers feeling loved. “I was spoiled by my brothers, that’s for sure,” she says.
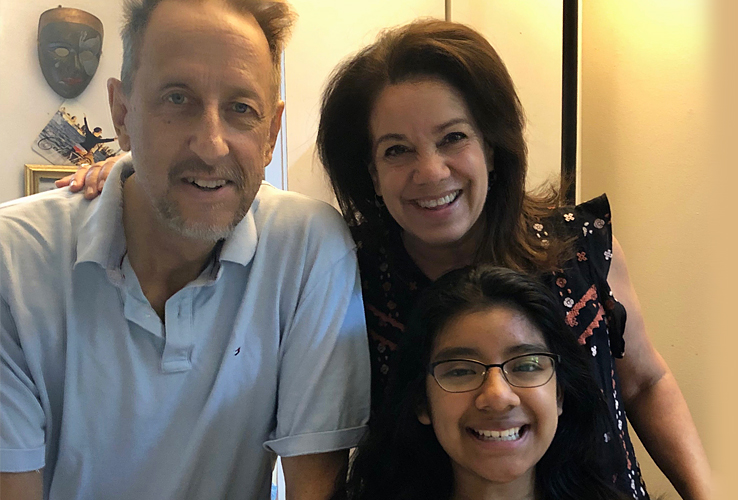
Like many siblings, she and Duncan drifted apart over the years. As an adult, he settled in Piermont, New York, with his wife, Gabriela, and 15-year-old daughter, Maya, where he runs a teleprompting business. Kim moved across the country to White Salmon in Washington state, where she is a home healthcare aide and mother to two boys in their 20s, Tai and Makani, and a 9-year-old girl named Aiyana. Both Kim and Duncan say they didn’t see each other as much as they would have liked.
A One-in-a-Million Diagnosis
Duncan began feeling tired and run down in November 2008. He assumed it was the flu—after all, he’d just had a normal checkup. But when he went in for a blood test after the new year, he received shocking news: “My doctor told me I was in kidney failure and that I had to get to the ER immediately,” Duncan recalls. His creatinine level—a waste product in the blood that kidneys normally remove and is one measure of how well the kidneys are functioning—was at 8; a healthy level is 0.5 to 1.5.
Dr. Jae Chang
“Normally, the kidneys filter creatinine from your blood, but when they aren’t working, it accumulates in your blood,” explains Dr. Jae Chang, Duncan’s current transplant nephrologist at NewYork-Presbyterian/Columbia University Irving Medical Center.
Before coming to NewYork-Presbyterian/Columbia, Duncan was diagnosed with anti-glomerular basement membrane (anti-GBM) disease, a rare autoimmune condition in which the body develops antibodies that attack the kidney. “No one knows what causes it,” says Duncan. “The doctors told me my chances of getting this were one in a million.”
His doctor predicted that his kidneys wouldn’t recover and said he should be placed on the waiting list for a kidney transplant—a list nearly 100,000 people long. But getting a kidney from a living donor was also an option. Living donors are able to donate a kidney to help those in need, so Duncan called his brother Randal to see if he might be willing to donate. His other brother wasn’t able to donate and Duncan didn’t think of asking Kim. Since they were not biologically related, both assumed she wouldn’t be a match. “It never crossed my mind that I could be a donor,” Kim says.

Dr. Lloyd Ratner
A Misconception About Organ Donation
Duncan and Kim’s assumption—that donor and recipient have to be a perfect match—is a common one. It is also incorrect. “With immunosuppressant drugs to prevent rejection, if you take any random pair of individuals, two-thirds of them will be compatible,” says Dr. Lloyd Ratner, director of the Renal and Pancreatic Transplant Program at NewYork-Presbyterian/Columbia and professor of surgery at Columbia University Vagelos College of Physicians and Surgeons. Dr. Ratner is also the current president of the American Society of Transplant Surgeons.
Getting a kidney from a living donor is generally preferable. “Besides bypassing the waiting list, with a living donor, the transplanted kidney will almost always work from the get-go,” says Dr. Ratner. “In contrast, a kidney from a deceased donor may take some time to ‘wake up.’ Then we have to put the patient on dialysis for a while, which means more days in the hospital and more potential complications.” With a living donor, the long-term outcome is typically better too. A kidney with a living donor lasts about 20 years, on average, twice as long as one from a deceased donor.
While Randal began the process to test for compatibility, Duncan went on hemodialysis at a center near his home, spending four hours three days a week to flush the toxins out of his body. “It wiped me out so badly that I fainted in a restaurant,” he recalls. Duncan was hopeful, however, that once he started peritoneal dialysis, a gentler process he could do at home, the routine would be easier to tolerate.
It was, but after eight or nine months, a strange thing happened. Duncan’s creatinine levels began to drop, down to 2.9 or 3. “Everyone was shocked,” he says. “My kidneys were recovering.” So much so that he stopped dialysis and was taken off the transplant list. Relieved, he went on with his life and work, albeit not as energetically as before.
She did a beautiful thing, and I’m eternally grateful. Her eagerness to do this was evidence of a very pure love.
Duncan Chinnock
A Déjà Vu Experience
That all changed when Duncan’s flu-like symptoms returned in summer 2018. “My creatinine shot back up to 9, and we were playing a waiting game,” he says. “I figured I had eight extra years of health that no one expected. My time had run out.”
Once again, he went on hemodialysis, followed by peritoneal dialysis at home. Once again, he reached out to Randal about donating, who, now 10 years older and in his mid-60s, felt some hesitation. Duncan then called Kim, wondering if she might be interested. “But I definitely thought of it as a Plan B,” says Duncan. “I figured she wouldn’t be a good match, or at least not as good a match as Randal.”
Kim had no such doubts. “I said, ‘Hell, yeah! Just tell me what I need to do,” Kim recalls. Her response was so whole-hearted and enthusiastic that Duncan called her back a few days later. “That’s when I told her, ‘I’d really love it if you could be the donor.’”
An Unlikely Match—or Maybe Not
Most people would be nervous about donating a kidney—after all, there’s the anesthesia, the surgery, the fear that maybe the transplant won’t work. Kim’s main worry, however, was that she wouldn’t be a match for her brother. She also had some concerns about what would happen if one of her three children needed a kidney down the line. “I took a few days to pray about it, but after digging deep, I realized that, hey, by the time my kids needed a kidney, I’d be too old to donate! After that, I felt totally at peace.” When Kim discovered that her blood type was 0—the universal donor, and compatible with Duncan—she was ecstatic. “I mean, this was for Duncan, my brother. It was a no-brainer.”
The first important factor for compatibility is blood type, followed by whether a donor has any antibodies against the recipient. “If you’ve ever been pregnant, had a blood transfusion or had any kind of transplantation, including a tissue graft, you might have antibodies,” Dr. Ratner says. “The third level is tissue matching, where we look for a match of antigens. It’s better if you have a higher degree of matching, but even if you don’t, you still can be a good donor.” For instance, a younger donor who is less of a match might be a better option than an older donor with more matching antigens.
Once Kim was deemed compatible on all these levels, in spring 2019 she began working with the transplant team at NewYork-Presbyterian/Columbia, where Duncan hoped to get his transplant. They arranged for Kim to get more tests near her home, including a mammogram, colonoscopy, and Pap test. “A potential donor doesn’t have to be in perfect health, but we do put people through an extensive evaluation to make sure everything will be as safe as possible,” says Dr. Ratner. A few issues that might preclude someone from being a donor: having diabetes, high blood pressure, certain transmissible diseases like HIV or hepatitis, or a history of cancer.
“But everyone should still sign up to be a donor—we can figure things out on the other side,” says Dr. Kasi McCune, a transplant surgeon at NewYork-Presbyterian/Columbia and an assistant professor of surgery, Division of Kidney and Pancreas Surgery at Columbia University Vagelos College of Physicians and Surgeons. “And for living donors, we tell people to check it out, even if you have doubts. We like to say that at least you’ll get the best checkup of your life. Often, we find things we wouldn’t have found otherwise, and patients can take care of them.”

Dr. Kasi McCune
In May 2019, Kim traveled to New York City for two more days of rigorous testing, including a CT scan, X-rays, and a stress test. Duncan went through his own series of tests, both siblings now under the care of the team at NewYork-Presbyterian/Columbia. Kim met Dr. Ratner, her surgeon, as well as a social worker, a coordinator, and a psychiatrist. “We want to make sure potential donors aren’t being coerced and that they understand what they are getting into,” says Dr. Ratner.
Kim sailed through, though being at the hospital was a bit surreal. “I felt like, ‘Oh my God, this is really happening,’” she says. Adding to that sense of disbelief was the fact that Kim had no idea what the doctors might find. “When you’re adopted and have no family history, you’re in the dark,” she says. “I just crossed my fingers and prayed there would be a good result.”
Duncan was also on tenterhooks, hoping that, if all went well with Kim, a transplant could happen by mid-summer. “It was tough waiting because dialysis was a grind,” he says. But once he and his wife met with his surgeon, Dr. McCune, his anxiety eased. “We were thrilled,” he says. “Dr. McCune was calm, a straight shooter, and clearly a rock star in the department.”
Dr. McCune was equally optimistic. “Many of our transplant patients also have diabetes or high blood pressure, but Duncan’s blood vessels were nice and healthy. That makes the surgery a joy to do, because we know we are going to get a good outcome.”
On August 13, 2019, both Kim and Duncan were wheeled into adjacent operating rooms on the third floor of NewYork-Presbyterian/Columbia University Irving Medical Center. What lay ahead: five or six hours of surgery, with the donor going first. In Kim’s case, the plan was for Dr. Ratner to remove her kidney with a minimally invasive technique known as laparoscopic nephrectomy, which he and a colleague were the first in the world to perform in 1995. “Compared with open surgery, patients recover faster,” he says.
Once Kim’s kidney was excised, the blood was flushed out, to prevent clotting, then the kidney was packed in slushy ice bags, covered with a sterile sheet, and wheeled across the hall, where Duncan was waiting.
Dr. McCune then picked up the baton, placing the new kidney—“about the size of a pocketbook,” she says—in Duncan’s abdomen. “The abdomen is more accessible to the bladder, which makes things easier,” she explains. Duncan’s own two kidneys were left in place. They would eventually stop working completely, then “shrivel up to the size of walnuts,” she says.
What happened next seems almost miraculous, even to seasoned surgeons like Drs. McCune and Ratner: “The new kidney started working immediately,” says Dr. McCune. Indeed, by the end of that first night, Duncan’s kidney had put out 6 to 10 liters of urine, removing the toxins that had built up in his body. “Most people urinate about 1½ liters a day,” says Dr. McCune. “But when we put a healthy kidney into someone with renal failure, it goes crazy.”
Duncan wasn’t initially aware of what was happening. Instead, his concern was for his sister. “I’m told that the first thing I asked when I woke up was, ‘How’s Kim doing?’” he recalls. Kim was feeling well enough to take a walk down the hall to Duncan’s room the day after surgery, trailed by her IV pole and Aiyana and Makani. “I wanted my kids to be a part of the experience,” says Kim. “I want them to be able to share the fact that I donated a kidney—and let people know that it’s good to donate if you can.”
Indeed, Kim was out of the hospital after two nights, and back to work within a month. Duncan’s recovery was equally swift. “I had every confidence in Dr. McCune, which was borne out on the day of surgery,” says Duncan. “It couldn’t have gone better. I’m just really grateful to Dr. McCune and the whole team.” He was out of the hospital in four days, his creatinine down to 1.2, a healthy level. And while rejection of the kidney occurs in 10% to 15% of cases, “it’s reversible with medication 99% of the time,” says Dr. McCune. After a year, the chances of rejection drop dramatically, though Duncan will continue to return for regular checkups with his transplant nephrologist Dr. Chang and will take immunosuppressant drugs for the rest of his life. But a mere four weeks after the transplant, he was also back at home, getting back to work, and enjoying time with his family.
I feel incredibly blessed that I got adopted by an incredible family. And I’m just so thankful that I could give that gift back.
Kim Chinnock
Yet life is also decidedly different, for both Kim and Duncan.
“It’s just a pleasure to finally feel good,” Duncan says. “I feel less weighed down, less lethargic, and clearer in my head. I feel healthy now. That’s the only way to describe it.” For that, he gives thanks to his entire care team, and, of course, to Kim. “She did a beautiful thing, and I’m eternally grateful,” says Duncan. “Her eagerness to do this was evidence of a very pure love.”
Duncan and Kim’s father, Frank, who died in 1981 at the age of 55, predicted Kim’s pure love—and her willingness to give to her brother Duncan. As Frank wrote in Kim: A Gift From Vietnam, his 1969 memoir of Kim’s adoption and first year with the family, “[Duncan] was her companion and her idol, for he had always been the one who took the time to play with her and who had the patience to stick with her through her tantrums. … She followed him everywhere. Her love for him was undiluted. She gave it to him without strings, a gift of the heart.”
Yet if you ask Kim, she’ll say that she is the one who has been given a gift—two gifts, in fact. “The fact that Duncan is here, that he can enjoy his life, that he can see his daughter graduate from high school, that’s all I care about,” she says, her voice catching. “I feel incredibly blessed that I got adopted by an incredible family. And I’m just so thankful that I could give that gift back.”
This piece was written by Duncan and Kim’s sister-in-law, Paula Derrow, a regular contributor to Health Matters.