Helping Puerto Rico’s Overburdened Medical System
A second disaster response team relieves the first group, who recently returned from a two-week mission.


Four weeks after Hurricane Maria hit, millions of people in Puerto Rico were still without access to food and water. Eighty-three percent lacked power. Cell phone service was limited, and many roads were blocked.
The impact on the island’s healthcare system was just as great, with medical care hampered by transportation issues and a 24/7 need for generators. There were fears of outbreaks of waterborne diseases.
To help provide much-needed medical care for suffering residents, NewYork-Presbyterian deployed a Disaster Response Team to the area on October 12. The four physicians and eight nurses were among 78 healthcare professionals who traveled to Puerto Rico as part of an effort coordinated by the Greater New York Hospital Association and the Healthcare Association of New York State, under the auspices of the U.S. Department of Health & Human Services, the State of New York, and the Puerto Rico Department of Health.
“The team was incredibly energized,” Jeffrey Bokser, vice president, Safety, Security & Emergency Services, NewYork-Presbyterian, said of the group, the first of two teams to travel to Puerto Rico. “It was just inspiring to see the passion, the dedication, the excitement to want to help, to want to go and make a difference.”
The first Disaster Response Team, led by Dr. Chris Tedeschi, an emergency medicine physician at NewYork-Presbyterian/Columbia University Irving Medical Center with extensive experience in disaster management, treated walk-ins and inpatients at one of the island’s federal medical shelters, “because there are a lot of clinics and doctors’ offices that obviously either closed or no longer exist because they’ve been destroyed. We anticipate those patients are coming and will be treated by our team,” Bokser says.
In addition, NewYork-Presbyterian donated $1 million to New York Healthcare’s Puerto Rico Hurricane Relief Fund to assist hospitals, healthcare workers, and their families in Puerto Rico and other Caribbean islands affected by the recent hurricanes. A trustee on the hospital’s board donated another $1 million.
NewYork-Presbyterian also sent medical supplies and emergency items, donated by patients and employees, to the island.
“When it comes to emergencies and emergency preparedness there is no better team, no one more capable than our team at NewYork-Presbyterian,” says Bokser. “We have employees who have tremendous experience in helping others, in responding in disaster situations. We received over 700 names of volunteers when we put out the message asking for people to help in Puerto Rico. We went through those 700 names and really had to come up with those individuals who we felt would be best suited to work in the environment and conditions down in Puerto Rico.”
On October 24, members of NewYork-Presbyterian’s second disaster response team boarded a plane bound for the island, along with dozens of other healthcare workers from throughout the state, for a two-week deployment.
The new team of 14 — four doctors, seven nurses, two physician assistants, and one liaison — is being led by Dr. Pia Daniel, an attending physician in the emergency department at NewYork-Presbyterian/Columbia University Irving Medical Center.
Once Team 2 arrived in Puerto Rico, they received their assignment: Providing around-the-clock care at the same federal shelter in Manatí, a city on the northern coast of Puerto Rico, where the first NewYork-Presbyterian team was based during its time on the island. (Team 1 treated over 2, 400 patients.) On Wednesday, October 25, the two NewYork-Presbyterian teams worked side-by-side at the shelter, allowing for a smooth transition before the first team returned to New York City the following day.
“The work that you are doing is so important, and on behalf of the whole hospital, we are so proud of you for the commitment that you are making,” Dr. Cam Patterson, senior vice president and chief operating officer at NewYork-Presbyterian/Weill Cornell Medical Center, told Team 2 before they left.
Dr. Tedeschi said the patients had inspired Team 1 during their stay. “Patients were hugging us on their way out the door, and we all were energized by their gratitude,” he said.
Dr. Shama Patel, an assistant attending physician in the Emergency Department at NewYork-Presbyterian/Columbia, echoed his thoughts. “They were the most resilient and wonderful people,” she said. “The people we worked with were amazing.”
In fact, it was the patients who had the most impact on some of the NewYork-Presbyterian team members.
They were “very thankful and very grateful,” said Nicholas Choi, a nurse in the Surgical Intensive Care Unit at NewYork-Presbyterian Queens. “So that was very reassuring and inspiring, rejuvenating for a healthcare provider, to be made to feel that way.”
Team 2 also has expertise in a range of specialties, including emergency medicine, disaster medicine, wilderness medicine, and pediatric care. Dr. Daniel, who specializes in disaster medicine, says the team is prepared and already has established roles. “Our real goal is to provide NewYork-Presbyterian–level care despite not being in New York,” she says.
Dr. Jonathan Lee, who is also an emergency department attending physician at NewYork-Presbyterian/Columbia, was eager to get on the ground and get to work. “This is what I feel most passionate about,” says Dr. Lee, who has completed an international emergency fellowship and has provided medical care in countries including Iraq, Egypt, and Ghana.
Emergency department physician assistant Nancy Pagan, who responded to the earthquake in Haiti in 2010 and has provided medical care in South American countries, expressed the same sentiment. “I love this kind of work,” says Pagan, who is based at NewYork-Presbyterian/Weill Cornell Medical Center. “And even though you may not have every resource needed at the moment, it just makes you a better practitioner because you’re trying to get answers with the little that you have.”
Pagan is also driven by her personal connection to Puerto Rico. She grew up there until age 12, and most of her family lives on the island.
Several team members have strong ties to Puerto Rico, including Dr. Susana Morales, attending physician in internal medicine at NewYork-Presbyterian/Weill Cornell Medical Center, whose grandfather came from Manatí. Nurse Erwin Perez is the first in his family not born in Puerto Rico. “It’s going to be an amazing opportunity for me to go help and serve down there,” says Perez, who works in the emergency department at NewYork-Presbyterian Brooklyn Methodist Hospital.
The deployments are part of an ongoing effort being coordinated by the Greater New York Hospital Association and the Healthcare Association of New York State, under the auspices of the U.S. Department of Health & Human Services, the State of New York, and the Puerto Rico Department of Health.
The members of both teams were “provided with sleeping bags and pillows appropriate for the climate in Puerto Rico and all the gear that they need to survive,” says Bokser. “We’ve given them meals ready to eat, water, and equipment to be self-sufficient.” Their backpacks included headlamps, goggles, bug spray, suntan lotion, and the ready-to-eat meals, including beef stew, beef stroganoff, and marinara sauce and meatballs.
Follow along with #NYPResponds for updates and read below about the team’s progress.
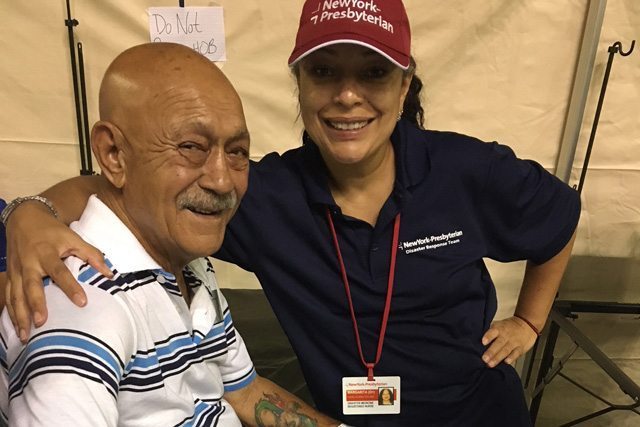
The NewYork-Presbyterian team on the ground in Puerto Rico.




Update: Thursday, October 12
After arriving in San Juan Thursday night, the team was moved the next day to Manatí on the northern coast, where it is working in a 150-bed federal medical center. The center is supported by FEMA and HHS, which are providing supplies and provisions to keep the shelter running. Team members are working around the clock and sleeping in shifts in a tent outside the unit. After about two weeks, the group will be replaced by another NewYork-Presbyterian team.
Update: Friday, October 13
On its first day, the team treated 205 adults and children, including 150 inpatients, many with waterborne illnesses and conditions related to dehydration. Eleven were more serious cases, and three were critical. Supplies, including sutures are in high demand, and after a short wait, HHS was able to locate a much-needed ultrasound machine, which is enabling the team to make accurate diagnoses.
“Not only are they providing clinical care, but the moment they arrived they brought a whole level of organization and efficiency and improvements to the quality of care on the ground,” says Bokser. “So things like coming up with care goals for patients, conducting medication reconciliation, putting a doctor in triage in the clinic areas where they have set up — things that we do routinely here, they’ve now established on the ground in Manatí. They were proud to share that. They brought what they described as ‘NewYork-Presbyterian style’ to Manatí.”
Update: Tuesday, October 17
The most common cases the team has seen are complications from diabetes and asthma, chest pains, and wounds people received while removing debris. In addition, they are treating cases not common in New York such as scorpion bites and a large number of what they believe to be leptospirosis from contaminated water. The team has been treating about 200 patients a day.
Update: Wednesday, October 18
After five days of treating patients, the 12-person NewYork-Presbyterian team has cared for close to 1,000 people who have come to the federal shelter. “Providers are starting to refer patients to our doctors at the site,” Bokser reports.
Update: Thursday, October 19
NewYork-Presbyterian’s emergency management team cared for about 200 patients at the federal shelter.
Update: Friday, October 20
It was another busy day for our NewYork-Presbyterian team in Manatí. Today, some of the team members helped to triage patients offsite at a nursing home that lost power and who needed to be evacuated. After returning from the nursing home, the federal medical shelter where our team is working also lost generator power for a period of time. They continue to adjust staffing along with the other clinicians to best meet the 24-hour-care needs. The team is treating skin abscesses, febrile gastroenteritis, and conjunctivitis, and is starting to see an uptick in respiratory infections.
Update: Saturday, October 21
The team left the federal center to do wellness checks in the community.
Update: Sunday, October 22
After a day without power and working with headlamps in Manatí, full generator power and air conditioning have been restored.
Update: Tuesday, October 24
Team 2 arrived in Puerto Rico and relieved Team 1, which returned to New York City the following day.
Update: Wednesday, October 25
Team 2 treated 198 patients today, its full first day in Puerto Rico.
Update: Thursday, October 26
The team treated 220 patients, and the daily census is expected to increase as transfers come from nursing homes unable to sustain operations and from the USNS Comfort, a Navy hospital ship. Shifts and responsibilities were divided for around-the-clock staffing.
Update: Friday, October 27
The number of patients coming to the shelter continues to increase, and the team treated 194 people today. The generators remain unstable, and team members often have to wear headlamps inside the shelter. Work is underway to try to connect the site to the power grid.
This morning, Dr. Shari Platt, a specialist in pediatric emergency medicine, and Dr. Zoltan Antal, chief of pediatric endocrinology, conducted the first peer-to-peer telemedicine consult for a 2-year-old with elevated blood sugars. The consult helped the team on the ground create a better discharge plan and adjust medications for the patient. It was successful and groundbreaking for delivering care in a disaster environment via a satellite dish.
Update: Saturday, October 28
The Manatí Federal Medical Shelter is now operating on the electric grid, and a local church is donating food for patients. Medications and pharmacy supplies are a challenge, and conservation is needed until new supplies arrive in a few days. The team is supplementing the federal government supplies with NewYork-Presbyterian provisions.
Members of the team were sent into the mountains to help transport two brothers with cerebral palsy for treatment in the shelter. A total of 207 patients —159 adults and 48 kids — were treated today.
Update: Sunday, October 29
The team treated 225 patients.
Update: Monday, October 30
Multiple providers from other teams have come down with viral illnesses. The NewYork-Presbyterian team gave flu shots to all inpatients at the Federal Medical Shelter. Dr. Joydeep Ghosh, a specialist in internal medicine, spearheaded this initiative and implemented protocols to try to stem the spread of illness among caregivers. Today, the team received a replenishment of needed supplies as well as additional staffing from U.S. Veterans Affairs.
Update: Tuesday, October 31
At the request of U.S. Health & Human Services and the Puerto Rico Department of Health, our team was split into two groups. Seven members stayed at Manatí, where they treated 198 patients, and six members were deployed to work on USNS Comfort, docked in San Juan. The ship is essentially a fully functioning hospital, and the team is staffing the emergency department under the direction of a U.S. Navy commander. It is also staffing a medical triage and urgent care tent on the dock with a disaster management assistance team. Healthcare needs are tremendous in San Juan, and patients are lined up for hours to seek care on the ship. The team expects to treat 250 to 300 patients per day. Dr. Pia Daniel brought Halloween costumes and candy for the team working in San Juan.
Update: Wednesday, November 1
The team in Manatí remains busy, as well. It treated 191 patients today and dealt with a power failure. Power was restored, but the shelter remains without air conditioning.
Update: Thursday, November 2
The team on the USNS Comfort is primarily assigned to staff the emergency department on the ship. However, our nurses and physician assistant assigned to the ship are also helping in the triage tent on the dock. The PA, Nancy Pagan, has already established a fast-track system on the dock, which has been well received, with hundreds of patients lining up daily for care.
The team in Manatí saw 191 patients today. Full power with air-conditioning has been restored. Influenza cases are beginning to grow, and the team is treating patients’ symptoms.
Update: Friday, November 3
The team saw 234 patients today. The Team 2 members on the USNS Comfort are now the only providers working the emergency department. Volume continues to be high on the ship and at the medical triage tent on the dock. On Monday, November 6, the ship will leave port to refuel. The team will come off the ship before it sets sail and work its remaining shifts in the medical tents on the dock in San Juan. It is seeing a lot of complications from chronic diseases and accidental trauma from infrastructure issues.
Update: Saturday, November 4
The Team 2 members still in Manatí spent the day assisting patients at a local hospital and preparing for its deployment tomorrow to San Juan. In San Juan, the team will work in a federal medical tent in the parking lot of the largest hospital in Puerto Rico. The team looks forward to establishing a footprint there for the duration of its deployment.
The other team members continue their work on the San Juan dock’s pop-up emergency department.
Update: Sunday, November 5
Team 2 said goodbye to Manatí today and was sent off with patients reading poems about the impact NewYork-Presbyterian had on their lives and families. The team is now operating in a tent outside of the hospital in San Juan. It is working with a disaster management crew from Minnesota and, inside a massive tent in the parking lot, is taking care of emergency department overflow patients from the hospital. The hospital is seeing 300 to 500 patients a day in the emergency department.
The team members on the dock continue their work in the urgent care tent in San Juan. All team members are in good spirits and excited about their mission for the remainder of the tour.

