New Hope in the Fight Against Addiction
Dr. Ronald Crystal aims to leverage the latest research to develop a vaccine that could curb cocaine dependence.
The notion of creating a vaccine to stop cocaine addiction came to Dr. Ronald Crystal nearly a decade ago, when he happened to pass a newsstand and noticed a magazine cover with the headline “The Hunt for an Addiction Vaccine.”
“I was a pulmonary physician. I knew nothing about addiction and had never been involved in the addiction field,” says Dr. Crystal, a pulmonologist at NewYork-Presbyterian/Weill Cornell Medical Center and chairman of genetic medicine at Weill Cornell Medicine. “But a lot of the research we were doing involved gene therapy, where we use viruses to transport genes into cells to fix diseases. I thought of that, and suddenly, I had an idea.”
It struck him that it might be possible to rely on the principles of gene therapy to develop a vaccine against cocaine addiction, the way inoculations put an end to smallpox and virtually eradicated polio.
In 2015, the latest year for which statistics are available, 6,800 people died of cocaine overdose, according to the National Survey on Drug Use and Health, a number that has grown steadily since 2012. And a 2011 report from the Drug Abuse Warning Network found that cocaine was involved in more than 500,000 of the nearly 1.3 million emergency department visits for drug abuse that year.
“Addiction is a major problem in this country and worldwide, and there are no good therapies for it,” says Dr. Crystal. Cocaine, in particular, is difficult to treat. “For heroin, we have methadone, but there is no drug available to treat cocaine dependency.”
Dr. Ronald Crystal
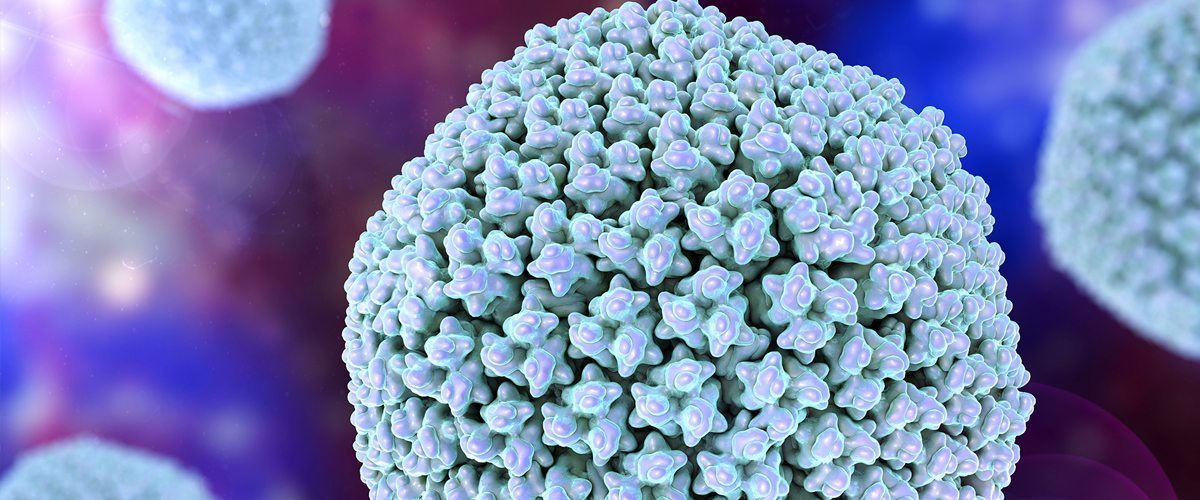
How a Cold Virus Might Cure Cravings
That may change, thanks to research Dr. Crystal is undertaking that looks at whether an experimental cocaine vaccine, invented by Dr. Crystal and his team and made with a common cold virus known as the adenovirus (pictured above), can cause active cocaine users to kick their habits.
“We know from our work that the adenovirus is very immunogenic — that is, it provokes a strong immune response,” explains Dr. Crystal. What that looks like in real life: If you’re riding on a bus and someone who has a cold with the adenovirus sneezes on you, you might catch the cold but your immune system will “see” the virus and develop antibodies against it.
“The next time you’re exposed to that adenovirus, you won’t catch a cold, because your immune system will generate even more antibodies against it and protect you.”
Knowing that process, Dr. Crystal and his team in the Department of Genetic Medicine at Weill Cornell Medicine came up with the idea of attaching an adenovirus to an “analog of cocaine” — a kind of drug decoy with the same characteristics as the street drug. The goal was to trick the immune system into thinking the cocaine look-alike was actually an adenovirus, and therefore trigger an all-out immune attack that would recur whenever cocaine subsequently entered the body.
In other words, once a person is vaccinated, the molecules of cocaine would become a target for antibodies, just like the adenovirus virus molecules are vulnerable to attack.
With the vaccine, the antibodies gobbled up the cocaine analogs like a little Pac-Man, neutralizing them before they reached the brain and produced a high.
Dr. Ronald Crystal
Normally, the body doesn’t produce antibodies against heroin or cocaine.
“That’s because these addictive substances are made up of very, very small molecules — so small that the immune system can’t ‘see’ them like they can see the larger molecules that compose the adenovirus,” says Dr. Crystal.
The new vaccine being studied might change that. Once the body is primed by the vaccine — consisting of the adenovirus attached to the cocaine analog — when trial participants use cocaine again, the hope is that their immune system will kick in, launching an attack against the drug as if it’s a common cold. Indeed, when the researchers injected laboratory animals with the vaccine, then gave them an intravenous dose of cocaine, the drug never reached the brain of the animals.
“It generally takes cocaine eight to 10 seconds to cross the blood-brain barrier. But with the vaccine, the antibodies gobbled up the cocaine analogs like a little Pac-Man, neutralizing them before they could reach the brain and produce a high,” says Dr. Crystal.
The patent for the anti-cocaine vaccine has been assigned to Cornell University and has not been licensed for commercial use.
Clinical Trials Happening Now
These animal experiments were so promising that they prompted Dr. Crystal and his team to launch in January 2017 a double-blind clinical trial of the vaccine with human subjects who actively use cocaine and want to quit.
Once participants are selected, researchers will administer a low dose of the vaccine. After the first vaccine, each person will receive a booster shot every four weeks for a total of six injections. Finally, each person will be monitored for three months, with weekly check-ins, until the end of the 32-week study. The entire phase 1 study is expected to take 1½ years.
“Each time the subjects come back — two or three times a week — we test their urine for the drug,” says Dr. Crystal. The plan is to start with 10 users. Seven will get the vaccine; three will get a placebo.
“I don’t know who is getting the vaccine and who isn’t, but the hope is that the people who do will use cocaine less than those getting the placebo,” Dr. Crystal explains, because they won’t feel the drug’s effects.
After the initial group of 10, Dr. Crystal and his team will test the vaccine and placebo on 10 more participants, then a final 10, for a total of 30 subjects. Each one will undergo standard drug dependency therapy throughout the study.
If Dr. Crystal’s trial with human cocaine users is successful, the hope is that this technology could potentially be applied to other addictive substances, such as nicotine or heroin, preventing the scourge of addiction all over the country and even the world.
“We’re thinking of it as a platform strategy,” he says. “We happened to start with cocaine, but if the concept works, we can start thinking about using it with a range of addictive molecules.”
For now, Weill Cornell Medicine and NewYork-Presbyterian/Weill Cornell Medical Center researchers are waiting to see how things evolve as they enroll more subjects and the results start rolling in. “We believe this is an innovative strategy to deal with a major societal problem,” says Dr. Crystal. “If it works, it will be a game-changer.”
