New Treatments for Gynecologic Cancer Patients
Dr. Jason Wright describes the cutting-edge advances in gynecologic cancers that are changing patient care.


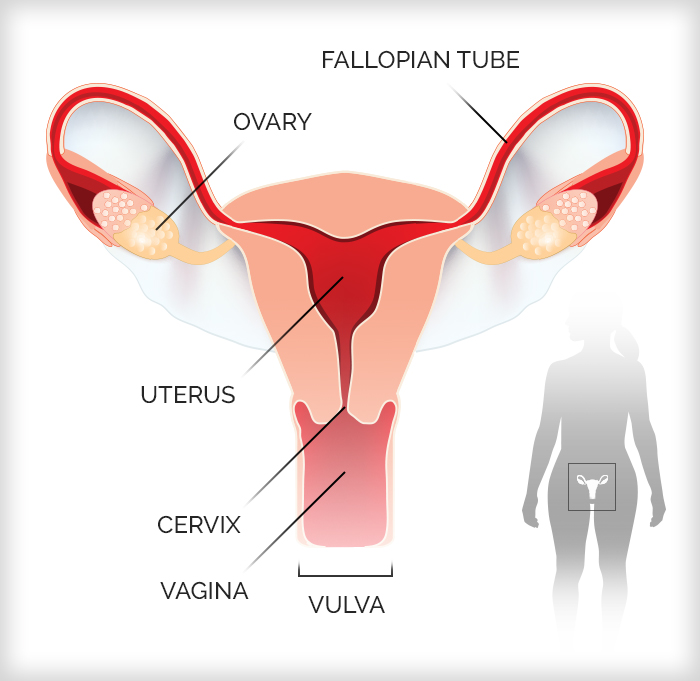
More than 116,760 new cases of gynecologic cancer were diagnosed in the U.S. last year, and 34,080 people died from these diseases, according to the American Cancer Society. Uterine (or endometrial), cervical and ovarian cancers are the most common, followed by vaginal and vulvar cancers.
Gynecologic cancers, which start in the reproductive organs, are often diagnosed at more advanced stages when treatments are less likely to work. The reproductive organs lie deep in the abdominal cavity, and symptoms are often vague, overlapping with common health complaints like digestive problems. Except for cervical cancer, there are no effective screenings to detect gynecologic cancers early.
But the outlook is improving for those who face these stealthy cancers. NewYork-Presbyterian is at the forefront of cutting-edge efforts to prevent and treat gynecologic cancers. Here, Dr. Jason Wright, chief of the Division of Gynecologic Oncology at NewYork-Presbyterian/Columbia University Irving Medical Center and vice chair of academic affairs, Department of Obstetrics and Gynecology at Columbia University Vagelos College of Physicians and Surgeons, shares with Health Matters the latest advances for people diagnosed with or at high risk for these diseases.
Hot Chemo
One new weapon against gynecologic cancer is hyperthermic intraperitoneal chemotherapy (HIPEC). It’s a highly effective way to deliver chemotherapy when ovarian cancer has spread to the lining of the abdominal cavity.
“We already had experience using this technology for other cancers at NewYork-Presbyterian/Columbia,” says Dr. Wright. “Now we’re able to offer it to women with ovarian cancer.”
How it works: A surgeon first removes all visible tumors in the abdomen, a process called cytoreduction. Then, while the patient is still on the operating table, doctors pump standard chemotherapy drugs heated to over 100 degrees directly into the abdominal cavity to target any remaining cancer cells.
“The idea is that we remove all of the cancer we can see and the HIPEC kills any microscopic areas of cancer inside the abdomen,” says Dr. Wright.
Patients are tilted up and down and side to side to disperse the drug to all surfaces of the abdominal wall. “Think of the abdomen as a bucket of water,” Dr. Wright says. “You’re turning it up and down and right and left and circulating the water around.” After about 90 minutes, the fluid is drained and the incision is closed.
Research shows the benefits. A study in the New England Journal of Medicine found that patients who received the treatment experienced a 12-month improvement in their overall survival compared to patients who only had chemotherapy administered through an IV.
HIPEC has several advantages over conventional chemotherapy regimens. For instance, the treatment allows doctors to use higher doses of the cancer-fighting agents. Heated chemotherapy may also be more effective at killing cancer cells.
Candidates for HIPEC must have cancer that is confined to the abdominal cavity and be fit enough to withstand a lengthy surgery and the potential risks of high-dose chemotherapy. “The cancer has to be completely resectable at the time of the surgery [meaning the tumor can be removed during surgery],” Dr. Wright says. “The treatment is also associated with greater toxicity, so the patient has to be younger and somewhat healthier before we do it.”
Hereditary Cancer Care
Up to 25% of ovarian cancers are caused by an inheritable genetic condition, such as a mutation in the BRCA1 or BRCA2 genes — the same genes that may raise breast cancer risk. People with a BRCA1 or BRCA2 gene mutation have about a 20% to 45% chance of developing ovarian cancer, compared to about 1% of women in the general U.S. population, says Dr. Wright.
The Hereditary Breast and Ovarian Cancer Program at NewYork-Presbyterian and Columbia University Irving Medical Center aims to improve the survival of women with such mutations. Launched in 2018, the program integrates the screening, prevention, diagnosis, and treatment of inherited breast and ovarian cancer, streamlining care. The program brings together experts from different medical specialties, offers genomic testing, and conducts clinical trials.
“The goal is to provide one-stop shopping for patients who either have one of these genetic abnormalities or may be at high risk for an abnormality,” says Dr. Wright. “For patients who carry a genetic abnormality, care usually involves going to a lot of different appointments for tests and to see different specialists. We’re trying to make it as easy and seamless as we can.”
The center’s patients tend to be from one of two populations. One group comprises people who have a family history of breast or ovarian cancer and want to find out if they have a genetic mutation that increases their risk for cancer. They may consult with a genetic counselor and undergo genetic testing.
The second group consists of those with a confirmed mutation who need help navigating their options. The options include enhanced screening, special imaging and blood tests to identify ovarian cancer, and prophylactic surgery — removing the ovaries or other reproductive organs as a preventive measure.
“Often when women have a family history of cancer, there’s a lot of fear around that association,” says Dr. Wright. “The goal of the center is to empower women, to give them as much information as possible, and then they can make informed decisions both for themselves and their family members.”
“The goal of the center is to empower women, to give them as much information as possible, and then they can make informed decisions both for themselves and their family members.”— Dr. Jason Wright
Personalized Treatments
NewYork-Presbyterian and its two affiliated medical schools, Columbia and Weill Cornell Medicine, are on the leading edge of precision medicine, a treatment approach tailored to individuals or certain groups of patients based on their unique characteristics. Through precision medicine programs, patients diagnosed with gynecologic cancers receive genetic testing, which helps to guide their treatment.
“Instead of treating all cancers of a given organ the same way, such as treating all ovarian cancers with one set of drugs or with one standard approach,” Dr. Wright says, “we’re now performing genetic testing and sequencing to look at the specific molecular abnormalities that are present in a cancer. We can then take these molecular abnormalities and design targeted treatments for women with gynecologic cancers.”
The approach can often dramatically extend survival and improve quality of life. “We’re able to offer patients new types of treatments and advances that may help extend their lives and hopefully increase their chance of curing the cancer,” Dr. Wright says.

Dr. Jason Wright
Groundbreaking Therapies
Breakthrough drugs, such as PARP inhibitors, are showing improved outcomes for people with gynecologic cancers. PARP is an enzyme that helps repair DNA damage. Drugs that block PARP prevent cancer cells from repairing themselves and cause cancer cells to die.
“These drugs are particularly effective for ovarian cancer,” Dr. Wright says. “Gradually there have been more and more uses for the drugs for people with ovarian cancer. For example, initially they were used for recurrent cases, and now they’re being used for people with ovarian cancer earlier, after their initial chemotherapy.”
Immunotherapy drugs are also showing promise in the treatment of gynecologic cancers, leading to significantly longer survival times. Immunotherapy helps the immune system mount a stronger defense against cancer.
“These are important drugs in our armamentarium,” says Dr. Wright. “We have seen patients who have had widespread disease, and they’ve received immunotherapy and had incredible responses that have been durable and lasting. That’s often unusual for the gynecologic cancers.”
Immunotherapy is used most often to fight cervical cancer. But increasingly physicians are using it to target other gynecologic cancers. “There’s a lot of emerging data now looking at ways to incorporate immunotherapy into the treatment of ovarian and uterine cancer,” Dr. Wright says.
A Surgical Technique to Reduce Complications
When oncologists remove a cancerous growth, they also take out nearby lymph nodes to see if the cancer has spread beyond the original tumor. This is needed to determine the stage of the cancer and guide treatment. But removing the lymph nodes can cause complications like lymphedema, which results in lifelong swelling and pain.
Now women with gynecologic cancers may be eligible for a node-sparing procedure called sentinel lymph node biopsy. “This has been around a long time for breast cancer,” says Dr. Wright. “But it’s now being used for gynecologic cancers, specifically uterine and vulvar cancers.”
Instead of removing all the lymph nodes in a given site, doctors inject a radioactive material (a colored dye) into a cancer, and then track where the dye goes, removing only the first lymph node that it drains to, called the sentinel lymph node. If that node is free of cancer, other nodes can be left in place.
“The hope is that we can get the diagnostic information that we need, but we can perform a less aggressive surgery,” Dr. Wright says. “So patients are hopefully at less risk for complications and side effects in the future.”
Additional Resources
Learn more about gynecologic cancer services at NewYork-Presbyterian.
Jason Wright, M.D., is chief of the Division of Gynecologic Oncology at NewYork-Presbyterian/Columbia University Irving Medical Center and vice chair of academic affairs in the Department of Obstetrics and Gynecology at Columbia University Vagelos College of Physicians and Surgeons. He is is a nationally recognized expert in the treatment of gynecologic cancers and gynecologic surgery. A major focus of Dr. Wright’s work is the delivery of quality care to women with cancer and the improvement of outcomes of women with cancer and those who undergo surgery. His primary clinical research focuses on the evaluation of novel therapeutics, targeted therapies, and biologic treatments for gynecologic cancers.