A Mom Donates Her Kidney to Save Her Daughter’s Life
When Lauren Shields underwent a heart transplant at age 8, her mother, Jeanne, never left her side. When Lauren needed a kidney transplant 12 years later, Jeanne calls her decision to become a donor a “no-brainer.”

Lauren and Jeanne Shields see each other for the first time post-transplant on July 23, 2020 (left) and visit a sunflower field in August 2020.
Last spring, amid the COVID-19 pandemic, Jeanne Shields felt helpless. Three times a week, she drove her daughter Lauren to a dialysis center near their home in Rockland County. Each time, Jeanne waited in her car outside as Lauren, with only a laptop and a knitted blanket to keep her company, spent three hours hooked up to a hemodialysis machine that did the work her failing kidneys couldn’t, cleaning the waste out of her blood.
“My body would be so drained after that. There were times I had to text my mom to come to the door and help me because I couldn’t walk out on my own,” says Lauren, then 20.
Jeanne wanted to sit with Lauren and hold her hand during the rigorous treatment — as she had done when Lauren recovered from a heart transplant in 2008 — but because of COVID-19 restrictions, she wasn’t allowed to accompany her daughter inside. “I cried every time I had to drop her off and send her in alone,” says Jeanne, 54. “That was devastating every single time.”
Adds Lauren: “It was the first time that we had ever been separated in my whole medical journey.”
Throughout Lauren’s life, her mother has always been her fiercest advocate and closest confidante. When Lauren was only 8 years old, she underwent a heart transplant at NewYork-Presbyterian Morgan Stanley Children’s Hospital, where Jeanne kept vigil every day. When Lauren became a young activist for organ donation, Jeanne drove her teenage daughter to Albany several times to share her story with New York State legislators. Since 2012, when Lauren’s Law passed in New York state requiring that people answer the question “Do you want to be an organ donor?” on all Department of Motor Vehicles forms, Jeanne has been celebrating the impact Lauren’s voice on increasing the number of new organ donor registrations throughout the state.

Jeanne and Lauren Shields have returned to boxing twice a week.
In fact, the only time the mother-daughter duo ever seem to spar is when they go to their local boxing studio to work out together twice a week. “We’ve always had an amazing relationship,” says Lauren. “My mom is my best friend.”
“We lean on each other when we need to,” says Jeanne. “She gets support from me, but I also get support from her.”
So, in January 2020, when doctors diagnosed Lauren with end-stage kidney disease and started talking about a possible kidney transplant, it came as no surprise that Jeanne was the first person to step up to become a living donor. “It was a no-brainer for me,” says Jeanne. “I spent so many years when she was going through her heart issue wishing I could do something to help her. I wanted to be the person that donated a kidney to her.”
Avoiding a Transplant at All Costs
Kidney disease is not uncommon for heart transplant recipients like Lauren, according to Dr. Warren Zuckerman, attending physician with the Program for Pediatric Cardiomyopathy, Heart Failure, and Transplantation at NewYork-Presbyterian/Columbia University Irving Medical Center and Lauren’s heart transplant cardiologist. “The main medication that we use to prevent rejection can unfortunately contribute to some kidney dysfunction,” says Dr. Zuckerman, who is also an associate professor of pediatrics at Columbia University Vagelos College of Physicians and Surgeons.
It also didn’t help that Lauren’s blood pressure had spiked. “The combination of high blood pressure and the effect of 12 years of anti-rejection medications that unfortunately can damage the kidneys exacerbated her kidney failure,” says Dr. Hilda Fernandez, a nephrologist at NewYork-Presbyterian/Columbia University Irving Medical Center and assistant professor of medicine in pediatrics at Columbia University Vagelos College of Physicians and Surgeons.
Still, when Lauren first heard her kidney diagnosis, she was optimistic that a transplant wouldn’t be in her future. “I was feeling great. My life was good. I still had energy and a good appetite. I was going to work out,” says Lauren, who was a sophomore at Dominican College at the time. “I didn’t think I needed another transplant.”
I remember walking into the operating room feeling like I was marching into battle with my fiery torch. I was just so excited to be able to help Lauren resume a normal life again.
Jeanne Shields
She did, however, make some lifestyle changes because “I was trying to avoid it at all costs,” she says. Lauren adopted a restrictive low-protein diet and increased her water intake. She also worked with Dr. Fernandez to adjust her medication to better manage her blood pressure.
Despite Lauren’s best efforts, her kidneys continued to decline at an alarmingly rapid rate. Over the next four months, Lauren would regularly be in and out of the hospital to manage her blood pressure, which would often register as high as 180/100. She was also becoming increasingly lethargic and losing weight.
By the beginning of May, Lauren had grown so weak that she couldn’t leave the couch and barely touched a meal. Jeanne insisted they go to the emergency room. Only this time when Lauren was admitted to NewYork-Presbyterian/Columbia University Irving Medical Center, her condition was so severe that she immediately underwent an emergency procedure to implant a dialysis catheter.
“I remember waking up from the procedure as they were rolling me into my room and the dialysis machine was already set up,” recalls Lauren. “The dialysis nurse was ready to go right then and there. I was barely awake. I was like, ‘Oh, my gosh, I can’t believe this is happening.’”
Meanwhile, even though Jeanne was a match for Lauren and eager to donate her kidney, a transplant wasn’t possible because most surgeries were postponed in New York City due to the coronavirus outbreak. That meant that Lauren had to endure dialysis for a while longer as COVID-19 continued to wreak havoc across the city.
“It was really hard to know that the kidney was right there in the room with me, yet I had to keep going through those dialysis sessions,” says Lauren.
She transitioned from inpatient dialysis to outpatient treatment three days a week, for 1 ½ hours at a time in the beginning. But as the weeks went on — and her kidney failure advanced quickly — her sessions got bumped up to two hours, then three. Sadly, Lauren only seemed to get worse.
“She was losing weight rapidly,” recalls Jeanne, who witnessed her daughter go from 84 pounds to a frail 64 pounds in a matter of weeks. “It was so painful to watch. It’s a horrible existence for anyone, but for a young girl who should be in the prime of her college days going out and having fun, it’s just not a good way to live.”
Meanwhile, all of Lauren’s qualms about undergoing a second transplant were no longer of concern. “When I was on dialysis, it got to the point that I thought, ‘I cannot do this anymore,’” says Lauren. “‘If a transplant is what is going to make me feel better and get me back to living my daily life, then I’ll do it.’”
[Lauren] was physically transformed, which is the miracle of a transplant.
Dr. Rodrigo Sandoval
The Heart of the Problem
Sadly, outpatient dialysis wasn’t cutting it. Lauren began retaining fluid, which put pressure on her heart. She was also having difficulty breathing due to fluid in her lungs. In mid-June, she was admitted to the ICU of NewYork-Presbyterian/Columbia University Irving Medical Center.
Figuring out why her heart function was deteriorating became critical in determining if she was still a viable candidate for a kidney transplant. “Initially, we didn’t know if the fluid buildup was from her heart or from her kidney failure,” explains Dr. Namrata Jain, a pediatric nephrologist and medical director of Pediatric Transplant at NewYork-Presbyterian/Columbia University Irving Medical Center.
To the relief of her care teams, they learned that Lauren’s heart was as strong as it was when it was transplanted 12 years ago. As it became clear that her deteriorating kidneys were putting extreme stress on Lauren’s body, a transplant became more urgent.
The pediatric kidney team worked closely with Lauren’s cardiology team to develop a vigorous four-week inpatient dialysis regimen that would strengthen Lauren’s heart and prepare her to receive her mother’s kidney. “The more aggressive inpatient dialysis was very helpful in improving her oxygen requirements, her respiratory distress improved, and her heart function improved,” says Dr. Jain, who is also an assistant professor of pediatrics at Columbia University Vagelos College of Physicians and Surgeons. This improvement in heart function helped pave the way to move forward safely with the kidney transplant.
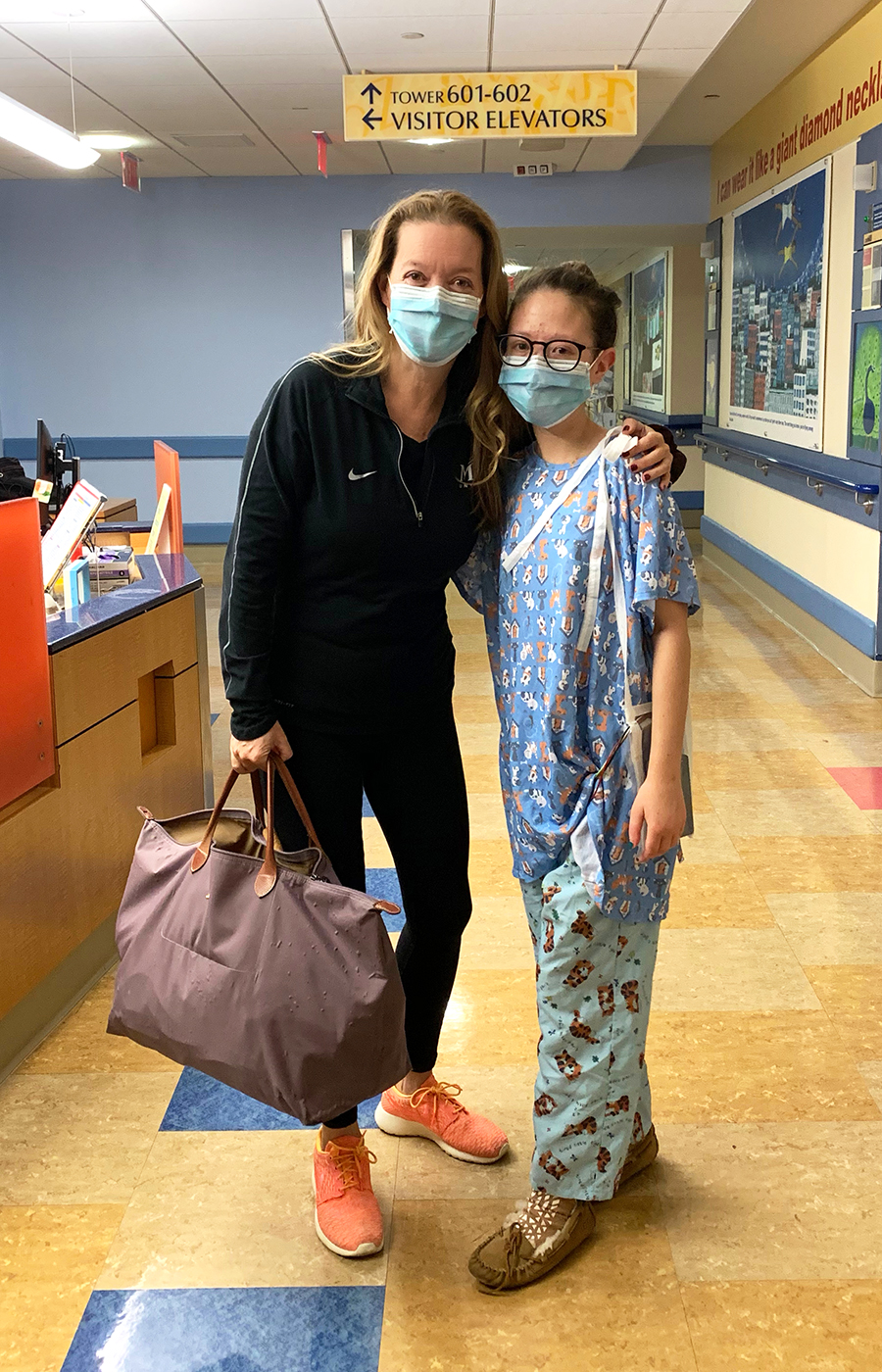
Jeanne and Lauren Shields on the morning of their transplant on July 21, 2020.
Finally, the day of the transplant arrived. At 5 a.m. on July 21, “I woke up so energized,” says Jeanne, who had never undergone a major surgery before. “I remember walking into the operating room feeling like I was marching into battle with my fiery torch. I was just so excited to be able to help Lauren resume a normal life again.”
Dr. Lloyd Ratner, director of Renal and Pancreatic Transplantation at NewYork-Presbyterian/Columbia University Irving Medical Center, removed Jeanne’s left kidney laparoscopically, a minimally invasive procedure that he pioneered and that has since become the standard of care throughout the world. Jeanne’s kidney was then carefully transported across the street to NewYork-Presbyterian Morgan Stanley Children’s Hospital where Lauren and Dr. Rodrigo Sandoval, associate director of surgical fellowship at NewYork-Presbyterian/Columbia University Irving Medical Center and Lauren’s kidney transplant surgeon, were waiting for the new organ.
Both surgeries went off without a hitch. “Jeanne is a very devoted mother who would basically do anything for her daughter,” says Dr. Ratner, who is also a professor of surgery at Columbia University Vagelos College of Physicians and Surgeons. “She was an excellent, healthy donor, and both Jeanne and Lauren’s surgeries went beautifully.”
“I woke up from surgery feeling amazing,” says Lauren, who went home two weeks post-transplant. “My skin and eyes were brighter. I couldn’t believe how fast I was able to walk around.”
Before the procedure, “Lauren was pale and gray like most people with advanced kidney disease. But she maintained her spirit. Even in the moments of suffering and pain, she managed to maintain humor and a positive spin on her health,“ says Dr. Sandoval, who is also an assistant professor of surgery at Columbia University Vagelos College of Physicians and Surgeons. “I saw her a few weeks later in the office, and she was physically transformed, which is the miracle of a transplant. She looked completely recovered — strong, beautiful, and happy.”
An Even Stronger Bond
Lauren, who turned 21 on April 13, is back to being a full-time junior studying health science, and she just completed the best semester of her college career thus far. “Since my transplant, I’ve had so much energy and can concentrate better,” she says, adding that she is interested in a career working with cardiac patients who have heart conditions like hers.
Jeanne, too, had a seamless recovery following her procedure. She was discharged after four days in the hospital and felt back to normal within two weeks. She has returned to working full-time as a real estate broker in Nyack, New York, and continues to go boxing with Lauren.
She also has a new passion: Promoting the positive impact of living organ donation. “When you give that gift, it’s such a wonderful feeling,” says Jeanne. “I talked to quite a few people who had donated kidneys, and everyone had the same response: They were so pleased with how quickly they got better, but most importantly, they were overjoyed with how the recipient was doing. Those are some of the best reasons to go forward and do it.”
Not a day goes by when Jeanne doesn’t feel grateful for being an organ donor for her daughter. “Any parent in my position would’ve done this,” says Jeanne. As a result, “our relationship only continues to get stronger.”
Lauren agrees: “We’re closer now — if that’s even possible.”
And now Lauren never has to worry about being without her mother again. “It’s surreal to be next to each other and to know that her kidney is inside of me,” says Lauren. “As hard as the whole situation was, especially with COVID, I feel so blessed and grateful that my mom was a match for me. I don’t know what I would do without her. She saved my life.”
Additional Resources
To learn more about becoming a living organ donor, visit nyp.org/organdonor or register to become an organ donor on registerme.org/nyp.
