The NewYork-Presbyterian Alexandra Cohen Hospital for Women and Newborns continues the hospital’s long tradition of being at the forefront of high-quality and compassionate care for expectant mothers and babies. From the founding of New York City’s first obstetrical hospital in 1799 to today’s modern-day facility delivering a personalized, best-in-class patient experience, here’s an overview of NewYork-Presbyterian and Weill Cornell Medicine’s rich history in maternal and neonatal medicine.
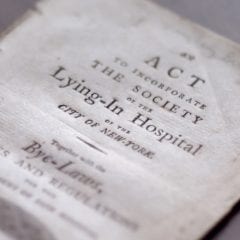
New York Hospital physician Dr. David Hosack founded the Lying-In Hospital of the City of New York after the yellow fever epidemic took a toll on expectant mothers. The Lying-In Hospital became the first obstetrical facility in New York City thanks in part to a $50 donation from Dr. Hosack’s renowned patient Alexander Hamilton. It remained open for a year before closing due to financial difficulties. The patients were then moved to New York Hospital (today NewYork-Presbyterian) on Broadway between what is now Duane and Worth Streets, where the Society of the Lying-In Hospital of the City of New York operated a maternity ward for poor women from 1801 to 1827.
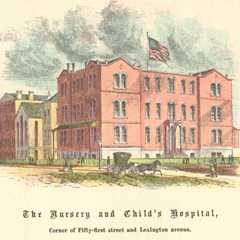
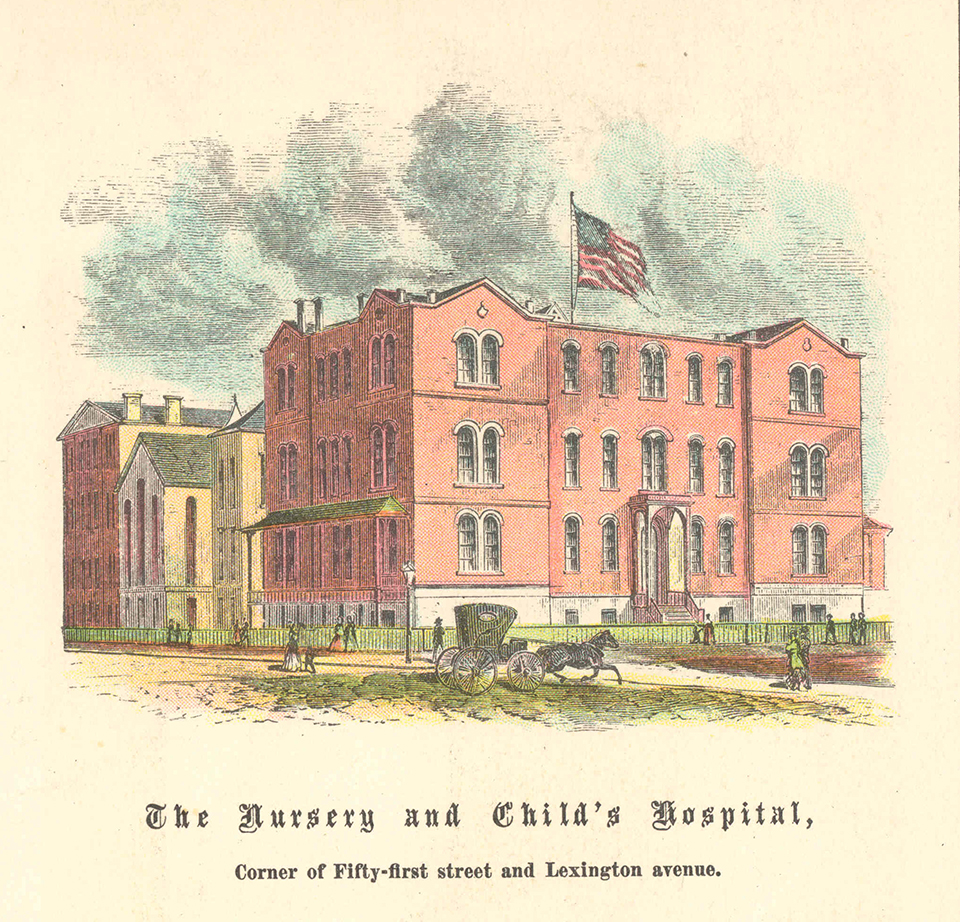
The Nursery for the Children of Poor Women opened on St. Mark’s Place as the first day care offering in New York City. The facility was meant for children of wet nurses and of parents who worked away from the home during the day. But the institution quickly shifted focus from day care to medical care of neglected and abandoned infants and underprivileged pregnant women. It later changed its name to the Nursery and Child’s Hospital in 1857 and moved to a larger location in midtown Manhattan where facilities for pediatric care and lying-in, the practice of giving mothers extended bed rest after childbirth, were added. In 1934, the institution was absorbed into what is now NewYork-Prebyterian/Weill Cornell Medical Center.
The Manhattan Maternity and Dispensary opened to care for women in confinement and operated as an alternative to city hospitals or at-home care. Both charity and paying patients were welcome, and a Social Service department offered mothers lessons in childcare. In 1932, the Manhattan Maternity and Dispensary merged into what was then the New York Hospital-Cornell Medical Center and became the hospital’s Pediatrics department.

A blood bank is established for blood transfusions in the Obstetrics and Gynecology department of New York Hospital-Cornell Medical Center, now NewYork-Presbyterian/Weill Cornell Medical Center. A year later an official Blood Bank, which is the first in New York State and second in the nation, is organized at the hospital.
Dr. George N. Papanicolaou, a pathologist at New York Hospital and an associate professor of anatomy at Cornell University Medical College (which became known as Weill Cornell Medicine in 2015), invented the diagnostic test known as the Papanicolaou (“Pap”) smear to detect the early stages of cervical cancer. As a result, the number of cervical cancer deaths in the U.S. declines dramatically.
The rooming-in plan is organized so mothers can have their babies with them overnight at New York Hospital-Cornell Medical Center (now known as NewYork-Presbyterian/Weill Cornell Medical Center).
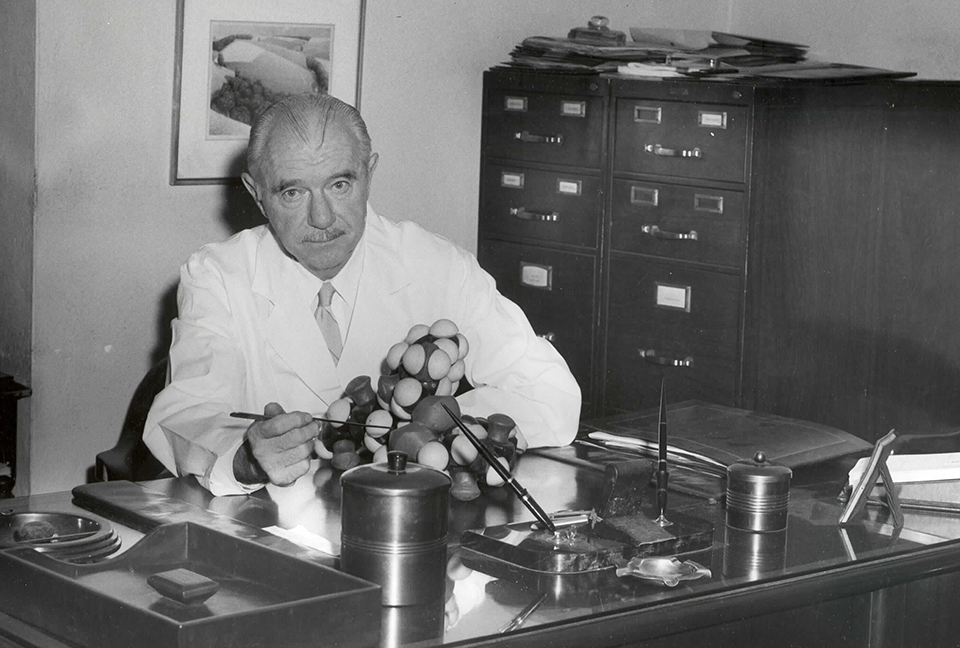
Dr. Vincent du Vigneaud, chair of the Biochemistry department at what is now Weill Cornell Medicine from 1938 to 1967, earned the Nobel Prize in Chemistry for his landmark research around oxytocin—a polypeptide hormone that is responsible for social bonding during sex, stimulating contractions during childbirth, and producing breast milk in women.
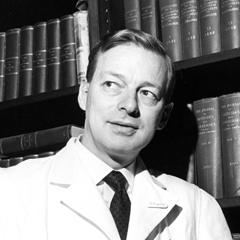
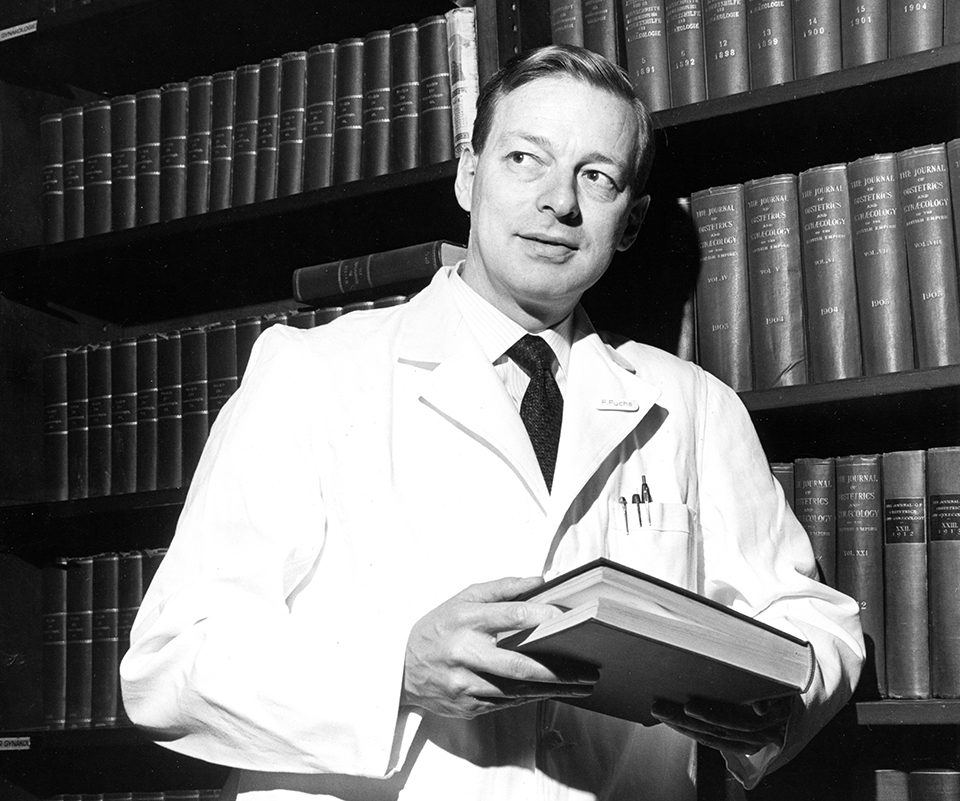
Dr. Fritz Fuchs, obstetrician and gynecologist-in-chief at NewYork-Presbyterian/Weill Cornell Medical Center from 1964 to 1978, is credited with being the first physician in the U.S. to use laparoscopy in gynecology, which is now widely utilized to diagnose and treat conditions related to women’s reproductive organs. He also advanced research on how to prevent premature labor alongside his wife, Dr. Anna-Riitta Fuchs, an endocrinologist and assistant professor in research at Weill Cornell Medicine.
The Perinatology Center opened its doors to high-risk mothers who need specialized care during pregnancy. It represented a joint operation between the departments of Pediatrics and OB/GYN at New York Hospital-Cornell Medical Center.
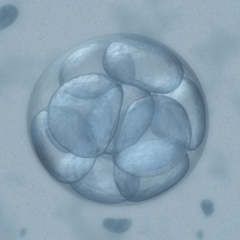
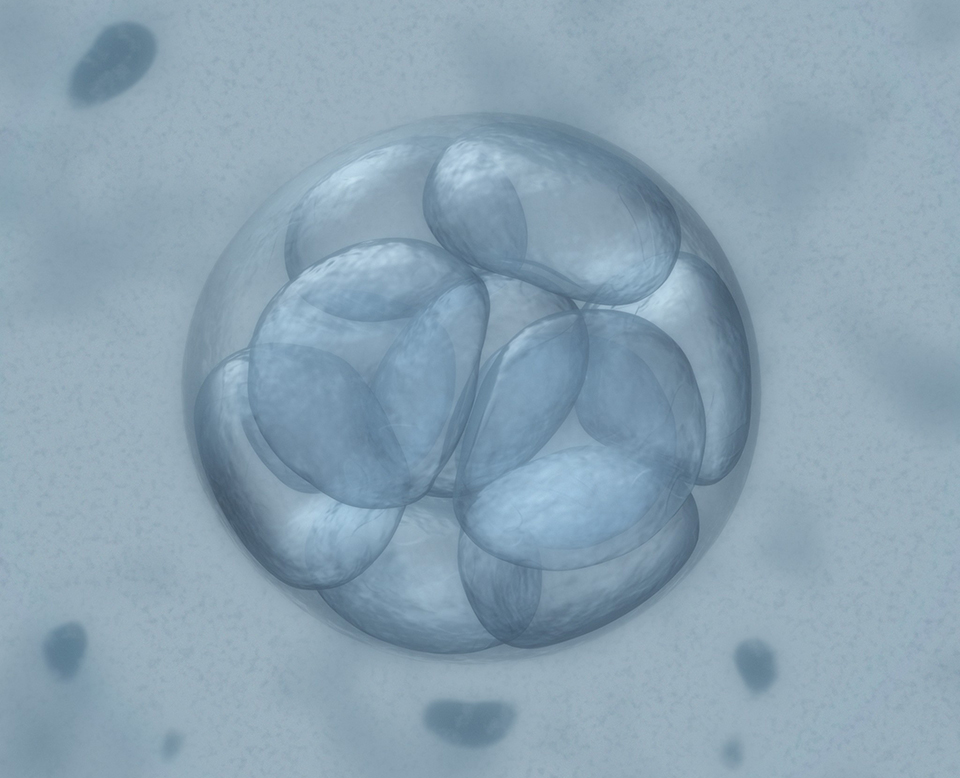
The first successful pregnancy and birth following an embryo biopsy (which is now widely referred to as a preimplantation genetic diagnosis) took place in the U.S. at what is now the Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine at Weill Cornell Medicine and NewYork-Presbyterian. The diagnostic technique, used in conjunction with in vitro fertilization (IVF), screens embryos for certain genetic diseases before implantation in the uterus, reducing the risk of parents passing on serious or fatal abnormalities to a child.
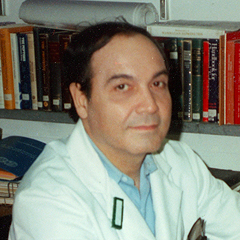
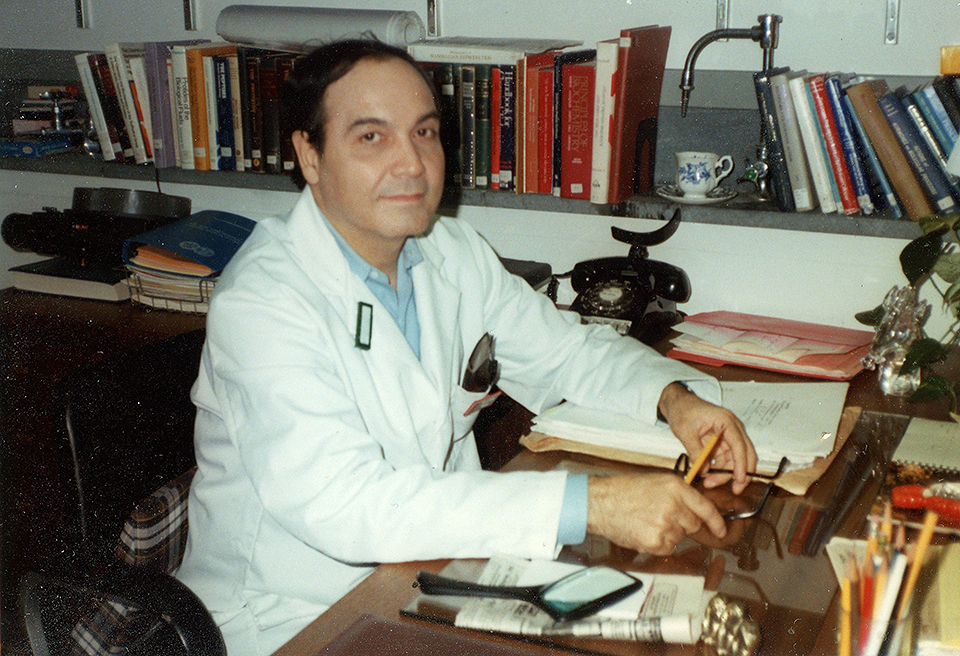
Dr. Zev Rosenwaks, director and physician-in-chief of the Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine at Weill Cornell Medicine and NewYork-Presbyterian and an obstetrician-gynecologist at NewYork-Presbyterian/Weill Cornell Medical Center, co-authored a study that discovered the anti-cancer drug tamoxifen boosts fertility and can help breast cancer patients have babies even after they experience fertility loss associated with chemotherapy.
A team of physician-scientists at the Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine obtained the first embryo from the frozen ovarian tissue of a breast cancer patient. The achievement increases the possibility for women and girls who undergo chemotherapy, radiation, or other ovary-damaging treatments to have their ovaries frozen in an effort to possibly restore fertility or reverse menopause at a later date.
The NewYork-Presbyterian Alexandra Cohen Hospital for Women and Newborns opens on the top six floors of the NewYork-Presbyterian David H. Koch Center. The state-of-the-art facility is dedicated to providing high-quality, individualized care to pregnant women and their babies before, during, and after childbirth—including advanced care for high-risk pregnancies. For newborns who require extra support, the new hospital’s Level IV NICU is the first in New York City to have a dedicated MRI and operating room within the unit.
Scroll to See NewYork-Presbyterian’s History