150 Days on the Front Lines
As July 29 marks the 150th day of NewYork-Presbyterian’s battle against the coronavirus, 10 healthcare workers reflect on the courage, fear, and hope they experienced in these unprecedented times.

On March 1, 2020, NewYork-Presbyterian diagnosed its first COVID-positive patient. Over the next four months — through the height of the coronavirus outbreak in New York City — the hospital cared for more than 17,200 patients who had contracted the virus.
As NewYork-Presbyterian marks the 150th day in its battle against COVID-19 on July 29, 10 front-line workers reflect on the harrowing, heroic, and heartbreaking experiences they witnessed. They describe the challenges they faced, the courage they summoned, and the love and hope that still keep them going as the pandemic rages on.
To hear more from these NewYork-Presbyterian heroes – and many more – visit My COVID-19 Story.

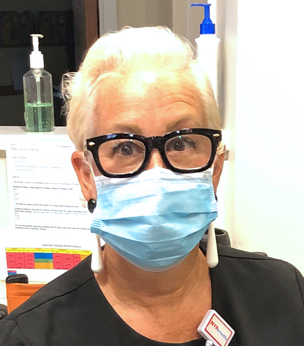
Valerie speaks about her experience caring for an influx of patients during the height of the COVID-19 crisis in New York City.
Valerie Louis, senior physician assistant, NewYork-Presbyterian Lower Manhattan Hospital
As patients continued to come in and we could not see a light at the end of the tunnel, my colleagues and I still came into work day-in and day-out without hesitation. We picked up overtime shifts and bent over backwards to do our part and then some.
To accommodate the influx, my unit expanded in ways I never thought possible. We changed structurally by adding beds. We changed operationally by adding members to the medical team (residents, intensivists, hospitalists), as well as staff who voluntarily answered the call to help from departments like Surgical Subspecialties Physician Assistants, Nursing, Respiratory Therapy, Environmental Services, Pharmacy and even Information Technology. All these changes allowed for us to increase our ability to care for these critically ill patients.
I work with an amazing team of supportive and dedicated physician assistants, doctors, nurses, patient care technicians, respiratory therapists, and patient relation specialists. We have always had each other’s backs — it’s the culture we’ve created in our work environment — so it’s no surprise that we supported each other even more once we entered this pandemic. We are built for this. I am built for this. Crises can bring out the worst and best in people, and I believe my entire ICU family brought their best to the workplace each and every day.

A senior accountant, Amr volunteered on the front lines during the coronavirus pandemic.
Amr Hassanein, senior accountant, NewYork-Presbyterian (volunteered at NYP Allen Hospital, NYP/CUIMC, NYP/WCMC, and NYP Lower Manhattan Hospital)
I saw so many parts of NewYork-Presbyterian during my time as a volunteer. At the Milstein Hospital Building, I was assigned to work with a patient transporter and I learned from him as we were transporting COVID patients around the hospital. I saw a lot of sick patients, but I kept myself in a healthy mental state by remembering my purpose there to help. It kept me optimistic.
In addition to my time as a transporter, I also distributed food to doctors and nurses, and worked in the kitchen and in the PPE Supply Chain Department. It was such a great opportunity to learn about the operational part of the hospital. I made lots of friends, and I was happy to come to work every day to learn something new.
I will never forget my time as a volunteer during the height of the crisis. It was inspiring seeing everybody in the hospital working together as one against this virus.

Dr. Mehta talks about how he found hope during his most difficult days while sick with COVID-19.
Dr. Parag H. Mehta, senior vice chairman of the Department of Medicine, NewYork-Presbyterian Brooklyn Methodist Hospital
My wife, daughters, and I are all COVID-19 survivors. During the weeks I was sick, I was able to reflect on my life. The adversities I faced have transformed me into a more positive person. I have found a new appreciation for life and the opportunity to help people as a physician. All the people who surrounded me while I was sick made me realize the amount of support, love, friendship, and care that cocooned me. Friends and family sent food, cleaning supplies, masks, and blessings.
While there were many days I had no appetite, when my daughters cooked for me I knew I had to try [to eat]. Food made with such love forced me to eat something. These acts of kindness continued when I returned to work. My colleagues and residents took care of me — making sure I was well hydrated, well fed, and staying healthy mentally and physically. This has made me even more committed to my work
In this time of uncertainty, there is one certainty: Love, support, and positivity are all around me.

Christine’s team helped train staff on safety measures and tracked every COVID-19 patient at NYP/Weill Cornell Medical Center.
Christine Hatola, infection control nurse, NewYork-Presbyterian/Weill Cornell Medical Center
The Infection Prevention and Control Department’s role during the crisis is to serve as the primary resource for best practices related to caring for COVID-19 patients and protecting our front-line workers.
I worked alongside four other infection control nurses and two epidemiologists to track patients as soon as they were admitted to ensure that they were immediately placed in proper isolation. At the beginning of the pandemic, it was so overwhelming to have about 40 new people come in each day with a highly transmittable disease that we didn’t have much data on because it was so novel. At the height of the outbreak, we were monitoring 400 admitted inpatients, including tracking over 200 patients who were critically ill and intubated.
For most of us, this pandemic has been the greatest challenge we’ve faced. The tireless effort, integrity, innovation, and teamwork within our team of nurses, physicians, data analysts, construction specialists, office assistants, and liaison observers are truly extraordinary. We simply could not have stepped up to meet this challenge without one another.

Renee quickly adapted to new roles and was awed by the compassion she witnessed.
Renee Lemieux, physical therapist, NewYork-Presbyterian Hudson Valley Hospital
The coronavirus has taken over, and like it or not, we are living in its midst. Our lives have changed radically, and, for every one of us, it means making an adjustment and being challenged by serious changes. For an outpatient physical therapist like me who has worked for the past two decades in orthopedic rehabilitation, it has meant suspending my patients for the time being and working in other capacities.
And yes, that means going to see patients with COVID-19.
What I witnessed one day when I joined the director of the Inpatient Rehab Department to assist with a patient in the Emergency Department will stay with me forever. This patient was seriously ill with COVID, and the director offered care with compassion, kindness, and gentleness. Her healing support toward the patient was truly remarkable. It will be marked as a powerful moment in my life — one that I won’t forget. Here I was nervous about a life-and-death situation for myself; there was the inpatient physical director treating our patient with the utmost confidence and expertise.
With unprecedented times come unprecedented changes, and from these changes come unexpected discoveries and precious moments like the one I witnessed in the Emergency Department.
Barbara shares how the COVID-19 hotline became a help line for people seeking care during an uncertain time.
Barbara Lowy, pediatric secretary, NewYork-Presbyterian Medical Group Queens
During the COVID-19 crisis, I was deployed to work the COVID Hotline in Queens. My responsibilities have been to schedule sick patients and employees with primary care physicians via telehealth or telephone.
But along with scheduling their much-needed appointments, I have also listened to their stories: people talking about their anxieties, new parents concerned about their babies, someone who had lost a family member, business owners concerned for their livelihood. The calls run the gamut of sadness. It is painful at times to hear their stories, but these are people’s lives and they are all delicate. I feel lucky that I can help in the slightest way, even if it’s just on the phone.
As we wrapped up each call, we say, “Thank you for choosing NewYork-Presbyterian for your care.” Most often the words I’ve spoken at the end are, “Please stay safe. Please take care of yourself. Please don’t hesitate to call us back.” Because it’s not just a hotline; it’s a help line really.
Zelenia saw strength, resilience, and love during the crisis.
Zelenia Felipe, medical-surgical oncology nurse, NewYork-Presbyterian Lawrence Hospital
As a medical-surgical oncology nurse for NewYork-Presbyterian Lawrence Hospital, I thought there was no bigger fight than cancer. Cancer was the “Big C” and something I helped my patients desperately fight every day. But a few months ago, we discovered another Big C: COVID-19. Having seen my patients fight cancer, I’ve learned the true strength of the human body and spirit. It’s that same strength and spirit that I know will not let COVID-19 win; the same strength and spirit that nurses carry every day as we walk into the hospital and put on our scrubs and PPE to begin our fight.
As I reflect on this time, I think of the team I have behind me, next to me, and in front of me on the front line of this COVID-19 battlefield. I think of every doctor, nurse, physician assistant, nurse practitioner, nursing assistant, patient care tech, patient advocate, physical and occupational therapist, pharmacist, pastoral care worker, social worker, case manager, dietitian, rapid response team, phlebotomist, lab tech, nutritionist, transporter, unit clerk, housekeeper, radiologist, respiratory therapist, pathologist, volunteer, environmental services staff, administration personnel, supervisor, and manager.
I think of them and the team we have built together over these past few months as we have all faced this challenge together. This battle would not have been fought at this rate had it not been for our teamwork and the work of our communities coming together to join us.

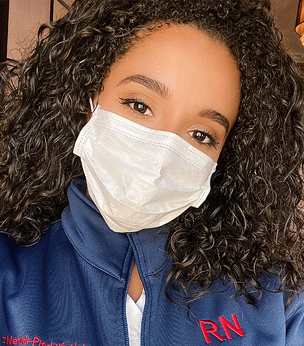
Sheera helped transform her unit to treat COVID-19 patients.
Sheera Gerber, registered nurse, NewYork-Presbyterian Westchester Behavioral Health Center
I don’t remember the exact date, but it was a Friday afternoon at around 2:30 when we were called into a meeting and were told that my unit would be converted into a COVID unit. At first, we felt scared because we don’t typically see acutely ill medical patients, so we had to obtain things like a reserve stash of PPE and learn the safety precautions.
Our staff really stepped up to the plate, going through our schedules to make sure that there were no holes and that there were regular faces there every day. We had to develop this new way of caring for these patients during a time that was constantly evolving. From the top down, the doctors stayed up to date on the research, they educated all the nurses, the nurses educated all the mental health workers, and we made sure to keep everybody knowledgeable. I’m proud of the way our unit has become a well-oiled machine, with the next person even more hardworking than the last.

Regina volunteered to work in the adult emergency departments when her colleagues needed her most.
Regina Kachkoff-Enk, emergency department nurse, NewYork-Presbyterian Morgan Stanley Children’s Hospital
With the pediatric population largely spared the worst of the COVID wave, I volunteered several of my shifts to help in the adult Emergency Department at NewYork-Presbyterian/Columbia University Irving Medical Center, just down the block. Later I also worked at the NewYork-Presbyterian Allen Hospital Emergency Department. As an ED nurse I’m used to seeing a large number of patients in distress, but this was far beyond what I had ever seen. It wasn’t just a lot of people. It was large numbers of people in severe distress, fighting to take in air. We had to constantly restock the oxygen tanks. Honestly, I don’t know what we would have done without our amazing respiratory therapists, not to mention the stockers and Environmental Services cleaning crews.
I am also a professionally trained opera singer, and I’ve been using my voice whenever the time has been right. I feel that music is always helpful in times of distress. It has a way of validating feelings of sadness and despair, and then lifting you out of them to a place of peace and joy. I have found myself listening to music more at this time, something I don’t do often enough. I’ve come to realize that I have the ability to make people feel better in more ways than one and have become less guarded with my own voice.

Brian tells his story of how he faced COVID at home, when a loved one fell ill, and at work.
Brian Gugliuzza, physical therapist, NewYork-Presbyterian/Columbia University Irving Medical Center
A news truck sits outside the energy court entrance on Broadway as the first cases reported in New York City become hospitalized here. Every employee moves at a slightly faster speed, and though you can feel a heightened sense of anxiety and alertness throughout the hospital, the hallways are eerily quiet. My phone rings – they have arrived for my family member’s daily radiation appointment, and because the usual entrance they use has been sealed off, I have to get a wheelchair because my relative is too tired to walk from Milstein to the service building. I have never seen my loved one more exhausted, and it concerns me.
As it was early on in the pandemic for New York, we assumed the fatigue was because of the daily dose of radiation to the head that my family member was receiving. But that day, my loved one had a temperature. They would be tested later at a fever clinic, and at the time, the two-day waiting period for a test result felt like forever. The test would be positive. I would call multiple times the night of the test results to make sure my loved one was OK. Inevitably, my family member developed shortness of breath. The next morning, I found out my relative’s status had deteriorated. My loved one was taken by EMS to a local hospital and would have to be intubated and placed in a medically-induced coma.
Nearly 18 weeks have gone by. My loved one has been weaned off of the ventilator but still requires a high flow of oxygen. There have been signs of progress, but by no means are they out of the woods. We remain in this never-ending state of fear, loneliness, and helplessness.
Despite all of this, there have been moments of grace and beauty. Every text, every phone call, every virtual hug temporarily brings a smile to my face. The future remains very unclear. Life is not fair. But life is beautiful.

For the full stories, plus audio and video, visit our My COVID-19 Story page.
