A New Patient Experience
Inside the NewYork-Presbyterian David H. Koch Center.
Imagine this: You’ve been diagnosed with an illness and fear the road ahead, assuming it will be stressful, confusing, and time-consuming for you and your family.
But then your primary care physician refers you to a specialist at the NewYork-Presbyterian David H. Koch Center. You make an appointment, fill out the paperwork online, and the day arrives. You’re a little nervous and not sure what to expect.
You arrive and walk into a light-filled lobby with a soaring ceiling. Someone greets you and helps you find your way. No lines. No waiting room with hard, uncomfortable chairs. No confusion about where you’re expected to be.
It’s about as close to a hospitality experience as a healthcare center can get.
Your patient ambassador has your information at her fingertips. She gives you a personalized smartband, allowing access to the building and alerting your care team of your arrival. Then, she directs you to the greeting area on the same floor where your treatment will take place. Another staffer shows you to your private prep and recovery room, where you will soon be met by your care team, who will tend to you throughout your stay — all on the same floor, in the same building, on the same day.
**
Before construction even began on the NewYork-Presbyterian David H. Koch Center — the new, state-of-the-art ambulatory care center on Manhattan’s Upper East Side — every decision was based on one thing above all else: the patient.
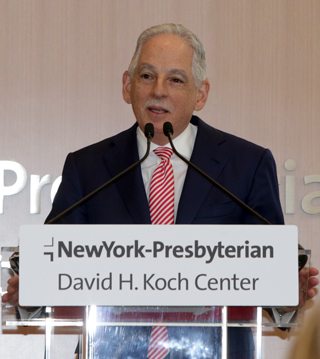
“Our goal in creating the NewYork-Presbyterian David H. Koch Center was to develop a new vision for what ambulatory care could be by focusing first and foremost on patients’ needs and the delivery of exceptional care,” says Dr. Steven J. Corwin, president and CEO of NewYork-Presbyterian. “Every decision about the design and operation of this building was made with the patient in mind, from the quick and easy check-in to the private prep and recovery rooms, light-filled treatment areas, and real-time status updates. This is truly an environment that was designed for healing, and we believe it represents the future of ambulatory care.”
The center is home to a wide range of ambulatory care services, including outpatient surgery, interventional radiology, diagnostic imaging, and infusion services, as well as an Integrative Health and Wellbeing program that will open in June 2018. And beginning in 2020, five floors will be transformed into the NewYork-Presbyterian Alexandra Cohen Hospital for Women and Newborns, offering best-in-class maternal and neonatal care. There is also a restaurant-quality cafe, comfortable lounge areas, and an underground parking garage offering valet service.
The road patients travel is not always an easy one, but it’s made much more comfortable — pleasant, even — by the center’s beautiful surroundings and high-tech amenities that place more power in patients’ hands.
“Susan Sontag wrote many years ago that … being sick is really like having two passports,” says Dr. Silvia Formenti, the Sandra and Edward Meyer Chair for Cancer Research, professor and chairman of radiation oncology, and radiation oncologist in chief of NewYork-Presbyterian/Weill Cornell Medical Center. “You have one passport when you’re healthy. You have another passport when you’re sick. As much as everybody wants to use the good passport, we all have times in our life when we’re holding the wrong passport. … NewYork-Presbyterian’s making it at least possible for the voyage to be very pleasant.”
Healthcare with Hospitality
“The building doesn’t necessarily feel like a hospital or a healthcare facility,” says Chif Umejei, the corporate director of information technology. “It has a bit of a hospitality feel to it.”
Natural lighting can be found throughout the building; there are no basement treatment areas here.
“There are a lot of studies that say natural lighting does improve care experience or the recovery experience,” notes Peter Stoffan, patient care director for pre-op and post-op services.
Other amenities help make the experience unlike any other in healthcare.
“Do you want really great food? You’re going to have it,” says Stoffan. “Do you really want a great nurse experience? You’re going to have a very small nurse-to-patient ratio. You’re going to have a lot of nursing aides and peri-operative patient assistants with you, ambassadors just really leading you. No matter what, we’re going to have the answers for you, and make you feel comfortable and safe.”
“Our goal in creating the NewYork-Presbyterian David H. Koch Center was to develop a new vision for what ambulatory care could be by focusing first and foremost on patients’ needs and the delivery of exceptional care.”— Dr. Steven J. Corwin
Patient as Partner
Every aspect of the NYP David H. Koch Center was thought through from the standpoint of the patient and their family and helping make their experience as stress-free as possible.
“The attention to detail is what sets this building apart,” says Kerri Hensler, patient care director of endoscopy, pre-PACU, and procedures.
“It was a true collaboration between our NewYork-Presbyterian staff and Weill Cornell Medicine as well as our patient and family advisory council, and our architectural and construction firms,” says John Simmons, director of operations and project management at the NYP David H. Koch Center.
Transforming the patient experience, making it more compassionate and efficient, is the raison d’etre for the NYP David H. Koch Center, and has been since its inception, because patients tend to have things in common regardless of what they’re being treated for: They’re generally anxious, stressed, and uncertain. None of that is good for healing. The center is designed to alleviate those stresses.
“If you think about where care is today, that’s not necessarily the case,” says Dean Caruso, director of hospitality services.
Through the NewYork-Presbyterian app, patients receive personalized information about their visit and step-by-step directions to their room, where their care team will greet them. Patients can also register their loved ones to receive real-time text updates about their care, while complimentary Wifi and an abundance of charging stations keep them connected.
And, when it’s time to go home, patients can easily access their discharge instructions, review test results, and even have a video follow-up appointment with their physician from home on their mobile device.
Coordinated Care
Here, streamlined care is the goal. Patients who are having a procedure have a home base — a private prep and recovery room where personal items may be left in a locker and your family can wait and receive updates on your treatment as well as enjoy the use of a computer tablet to help pass the time.
Even during treatment or surgery, you won’t be far from your loved ones, who can stay and use your room rather than a communal waiting area. The center was planned so that a multidisciplinary team of physicians from Weill Cornell Medicine, all working together under one roof, can provide coordinated care. This allows breast cancer patients and their family members or friends, for example, to see the surgeon, medical oncologist, radiation oncologist, and plastic surgeon without having to travel between crowded buildings or cross busy city streets.
“That’s the way we’re providing care,” says Cookie Frempong, director of outpatient oncology, “by bringing all the services to the patient.”
Top Technology
Throughout the building, state-of-the-art technology helps doctors diagnose and treat patients, and is another way NewYork-Presbyterian is working to improve the patient experience.
The center’s MRI/PET/Angiography suite is the first of its kind in the world. Combining all the key imaging technologies used for minimally invasive procedures, including MRI/PET, fluoroscopy, ultrasound, and rotational CT, the suite enables clinicians to diagnose, plan, and precisely guide procedures and verify their completeness. If, for example, it is determined that additional therapy is necessary to treat a tumor, that care can happen during the same visit. A first-of-its-kind patient table design enables use of all of these technologies without having to move patients from table to table or room to room.
“From a patient’s perspective, currently, you would have to go to three different places to get the same type of procedure that you can do in one room,” says Jean L. Aime, director of radiology and imaging, referring to the MRI/PET/Angiography suite on the fifth floor.
Equally notable is the center’s three linear accelerators, including New York’s first MRI-guided linear accelerator for precision radiation treatment of tumors. This leading-edge technology finds, targets, and tracks the position and shape of tumors while radiation is precisely delivered — a groundbreaking advancement in cancer treatment.
“The patient is in an MRI machine, so you can image the tumor in real time,” says Dr. Nicholas Sanfilippo, vice chairman of radiation oncology. “We can see if there’s any motion related to breathing or any other patient movement so that the radiation can be directed in the most targeted way possible.”
Caring For the Whole Person
Just breathe. It’s hard to do when you’re worried about your health.
But the Integrative Health and Wellbeing program at NewYork-Presbyterian, in collaboration with Weill Cornell Medicine, can help. The services are an effort to treat the whole patient, reduce anxiety, and enhance the patient experience.
Learn more about the NewYork-Presbyterian David H. Koch Center.
“Integrative health definitely is a supportive factor that we provide to our patients,” says Frempong. “They’re complementary services, so we will provide light massage, we will also provide Reiki, yoga, and also pre-op classes … that will help support their mind, body, and soul.”
“This building is a really unique opportunity to revisit the experience of being sick in a different context,” says Dr. Formenti. “It’s really shifting the balance from the disease to health. The disease becomes an episode and, of course, while working to make it go away, we try to transform the experience into just an episode that is somehow a fragment of the entire person — and keep the focus on health.”